Definition
Crohn’s disease is an inflammatory bowel disease (IBD). It causes swelling of the lining of your digestive system, which can result in stomach pain, extreme diarrhea, tiredness, effective weight loss and malnutrition. Swelling triggered by Crohn’s disease can include different areas of the digestion system in various people.
The swelling triggered by Crohn’s disease typically spreads out deep into the layers of impacted bowel tissue. Crohn’s disease can be both uncomfortable and debilitating, and sometimes might lead to deadly complications.
While there’s no recognized remedy for Crohn’s disease, therapies can significantly reduce its symptoms and signs and even cause long-lasting remission. With treatment, lots of people with Crohn’s disease are able to work well.
Symptoms and Signs of Crohn’s Disease
In some individuals with Crohn’s disease, just the last segment of the little intestinal tract (ileum) is influenced. In others, the disease is restricted to the colon (part of the large intestine). The most typical areas influenced by Crohn’s disease are the last part of the small intestinal tract and the colon.
Symptoms and signs of Crohn’s disease can range from mild to extreme. They generally establish gradually, but often will come on unexpectedly, without caution. You might also have amount of times when you have no signs or signs (remission).
When the disease is active, symptoms and signs might consist of:
- Diarrhea. Diarrhea is a common problem for people with Crohn’s disease. Magnified intestinal tract cramping likewise can add to loose stools.
- Fever and tiredness. Many individuals with Crohn’s disease experience a low-grade fever, likely due to swelling or infection. You may likewise feel tired or have low energy.
- Stomach pain and cramping. Swelling and ulceration can impact the regular movement of contents through your digestive system and may cause pain and cramping. You might experience anything from slight pain to severe pain, including nausea and throwing up.
- Blood in your stool. You may see bright red blood in the toilet bowl or darker blood mixed with your stool. You can also have bleeding you do not see (occult blood).
- Mouth sores. You may have ulcers in your mouth similar to canker sores.
- Decreased appetite and weight loss. Stomach pain and cramping and the inflammatory reaction in the wall of your bowel can affect both your cravings and your capability to digest and absorb food.
- Perianal disease. You may have pain or drain near or around the rectum due to swelling from a tunnel into the skin (fistula).
Other symptoms and signs
People with severe Crohn’s disease may also experience:
- Inflammation of skin, eyes and joints
- Inflammation of the liver or bile ducts
- Postponed development or sexual development, in children
When to see a medical professional
See your physician if you have consistent modifications in your bowel routines or if you have any of the symptoms and signs of Crohn’s disease, such as:
- Abdominal pain
- Blood in your stool
- Ongoing bouts of diarrhea that do not respond to over-the-counter (OTC) medications
- Unexplained fever lasting more than a day or two
- Unexplained weight-loss
Causes of Crohn’s Disease
The exact reason for Crohn’s disease stays unidentified. Previously, diet and stress were thought, but now doctors understand that these elements might intensify however don’t cause Crohn’s disease. A number of elements, such as heredity and a malfunctioning immune system, likely play a role in its advancement.
- Immune system. It’s possible that a virus or bacterium might activate Crohn’s disease. When your body immune system aims to battle the invading microbe, an abnormal immune reaction causes the body immune system to assault the cells in the digestion system, too.
- Genetics. Crohn’s is more typical in people who have relative with the disease, so genes may play a role in making people more vulnerable. However, the majority of people with Crohn’s disease do not have a household history of the disease.
Risk factors
Risk factors for Crohn’s disease might include:
- Age. Crohn’s disease can happen at any age, but you’re likely to develop the condition when you’re young. The majority of people who establish Crohn’s disease are diagnosed before they’re Thirty Years old.
- Ethnicity. Although Crohn’s disease can influence any ethnic group, whites and individuals of Eastern European (Ashkenazi) Jewish descent have the highest risk.
- Family history. You’re at higher risk if you have a close relative, such as a moms and dad, sibling or child, with the disease. As numerous as 1 in 5 individuals with Crohn’s disease has a member of the family with the disease.
- Smoking. Smoking is the most essential manageable risk element for developing Crohn’s disease. Cigarette smoking also leads to more serious disease and a higher risk of having surgery. If you smoke, it is necessary to stop.
- Nonsteroidal anti-inflammatory medications. These consist of ibuprofen (Advil, Motrin IB, others), naproxen salt (Aleve, Anaprox), diclofenac sodium (Voltaren, Solaraze) and others. While they do not cause Crohn’s disease, they can result in swelling of the bowel that makes Crohn’s disease worse.
- Where you live. If you live in a city location or in an industrialized country, you’re most likely to establish Crohn’s disease. This recommends that ecological factors, including a diet high in fat or refined foods, contribute in Crohn’s disease. Individuals living in northern climates likewise seem to be at greater risk.
Complications
Crohn’s disease may cause several of the following complications:
- Swelling. Inflammation might be confined to the bowel wall, which can result in scarring and constricting (stenosis), or might spread through the bowel wall (fistula).
- Bowel obstruction. Crohn’s disease affects the thickness of the intestinal tract wall. Over time, parts of the bowel can thicken and narrow, which might obstruct the circulation of digestive contents. You might require surgery to get rid of the infected part of your bowel.
- Ulcers. Persistent inflammation can lead to open sores (ulcers) anywhere in your digestive tract, including your mouth and anus, and in the genital area (perineum).
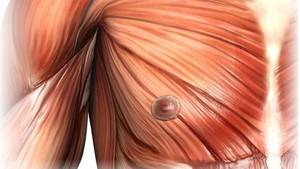
- Fistulas. Sometimes ulcers can extend totally through the intestinal tract wall, producing a fistula– an unusual connection in between different body parts. Fistulas can develop in between your intestine and skin, or between your intestinal tract and another organ. Fistulas near or around the anal location (perianal) are the most typical kind.
When fistulas establish in the abdomen, food might bypass areas of the bowel that are necessary for absorption. Fistulas might take place in between loops of bowel, into the bladder or vagina, or out through the skin, triggering constant drainage of bowel contents to your skin.
In some cases, a fistula may become contaminated and form an abscess, which can be deadly if not dealt with.
- Anal crack. This is a little tear in the tissue that lines the anus or in the skin around the anus where infections can happen. It’s often connected with uncomfortable bowel movements and might cause a perianal fistula.
- Malnutrition. Diarrhea, abdominal pain and cramping may make it hard for you to consume or for your intestinal tract to soak up sufficient nutrients to keep you nurtured. It’s likewise common to establish anemia due to low iron or vitamin B-12 brought on by the disease.
- Colon cancer. Having Crohn’s disease that affects your colon increases your risk of colon cancer. General colon cancer screening guidelines for individuals without Crohn’s disease call for a colonoscopy every 10 years beginning at age 50. Ask your medical professional whether you need to have this test done faster and more frequently.
- Other health issue. Crohn’s disease can cause issues in other parts of the body. Amongst these problems are anemia, osteoporosis, and gallbladder or liver disease.
- Medication threats. Specific Crohn’s disease drugs that act by blocking functions of the body immune system are connected with a little risk of establishing cancers such as lymphoma and skin cancers. They also enhance risk of infection.
Corticosteroids can be connected with a risk of osteoporosis, bone fractures, cataracts, glaucoma, diabetes and hypertension, among others. Deal with your doctor to determine dangers and benefits of medications.
Tests and diagnosis
Your physician will likely diagnose Crohn’s disease only after dismissing other possible causes for your signs and symptoms. There is no one test to diagnose Crohn’s disease.
Your medical professional will likely utilize a mix of endoscopy with biopsies and radiological screening to assist confirm a diagnosis of Crohn’s disease. You may have several of the following tests and procedures:
Blood tests
Tests for anemia or infection. Your doctor may recommend blood tests to check for anemia– a condition where there aren’t sufficient red blood cells to carry adequate oxygen to your tissues– or to check for signs of infection. Professional standards do not presently advise antibody or hereditary screening for Crohn’s disease.
Fecal occult blood test. You might need to provide a stool sample so that your medical professional can check for concealed blood in your stool.