Menorrhagia is the medical term for menstrual periods with abnormally heavy or extended bleeding which you can describe as ‘heavy menstrual bleeding with clots’. Although it is a typical concern, many women don’t experience blood loss severe enough to be specified as menorrhagia.
With heavy menstrual bleeding with clots, you can’t maintain your normal activities when you have your period since you have so much blood loss and cramping. If you fear your period due to the fact that you have such heavy menstrual bleeding, especially with blood clots, talk with your doctor. There are many reliable treatments for heavy menstrual bleeding.
Symptoms
Signs and symptoms of menorrhagia may consist of:
- Restricting everyday activities due to heavy menstrual circulation
- Symptoms of anemia, such as fatigue, fatigue or shortness of breath
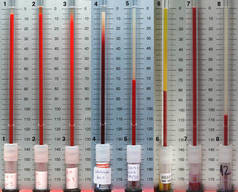
- Having to use double sanitary security to manage your menstrual circulation
- Having to awaken to change hygienic defense during the night
- Feeling bad for longer than a week
- Passing embolism larger than a quarter
- Soaking through several sanitary pads or tampons every hour for several consecutive hours
When to see a doctor
Seek medical aid prior to your next set up test if you experience:
- Vaginal bleeding so heavy it soaks a minimum of one pad or tampon an hour for more than two hours
- Bleeding between periods or irregular vaginal bleeding with blood clots
- Any vaginal bleeding after menopause
What Causes Heavy Menstrual Bleeding With Clots?
In some cases, the reason for heavy menstrual bleeding with clots is unknown, but a number of conditions may cause the issue. Typical causes consist of:
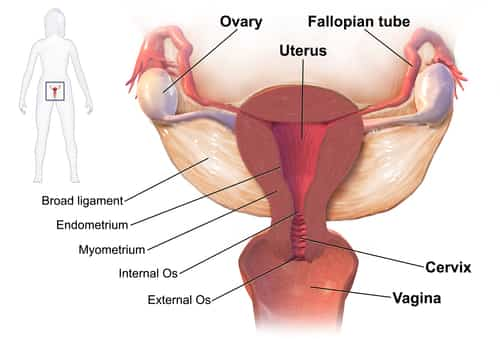
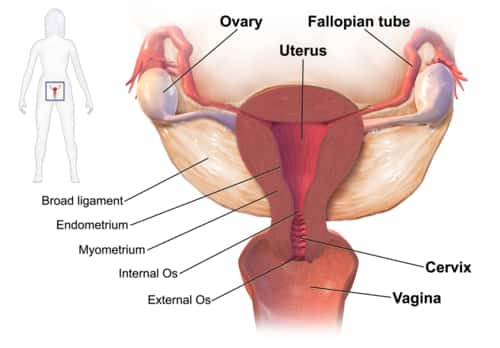
- Hormone imbalance. In a normal menstrual cycle, a balance between the hormones estrogen and progesterone manages the buildup of the lining of the uterus (endometrium), which is shed during menstruation. If a hormone imbalance takes place, the endometrium establishes in excess and ultimately sheds by method of heavy menstrual bleeding.
- A variety of conditions can cause hormone imbalances, including polycystic ovary syndrome (PCOS), obesity, insulin resistance and thyroid issues.
- Dysfunction of the ovaries. If your ovaries do not launch an egg (ovulate) during a menstruation (anovulation), your body does not produce the hormone progesterone, as it would during a normal menstrual cycle. This results in hormone imbalance and might result in menorrhagia.
- Uterine fibroids. These noncancerous (benign) tumors of the uterus appear during your childbearing years. Uterine fibroids might cause heavier than normal or prolonged menstrual bleeding.
- Polyps. Small, benign growths on the lining of the uterus (uterine polyps) may cause heavy or prolonged menstrual bleeding.
- Adenomyosis. This condition happens when glands from the endometrium ended up being ingrained in the uterine muscle, typically causing heavy bleeding and painful periods.
- Intrauterine device (IUD). Menorrhagia is a widely known side effect of using a nonhormonal intrauterine device for contraception. Your doctor will help you plan for alternative management options.
- Pregnancy complications. A single, heavy, late period may be due to a miscarriage. Another reason for heavy bleeding during pregnancy consists of an uncommon place of the placenta, such as a low-lying placenta or placenta previa.
- Cancer. Uterine cancer and cervical cancer can cause excessive menstrual bleeding with clots, particularly if you are postmenopausal or have had an abnormal Pap test in the past.
- Acquired bleeding disorders. Some bleeding disorders– such as von Willebrand’s disease, a condition where a crucial blood-clotting factor wants or impaired — can cause irregular menstrual bleeding.
- Medications. Specific medications, including anti-inflammatory medications, hormonal medications such as estrogen and progestins, and anticoagulants such as warfarin (Coumadin, Jantoven) or enoxaparin (Lovenox), can add to heavy or prolonged menstrual bleeding.
- Other medical conditions. A variety of other medical conditions, consisting of liver or kidney disease, may be connected with menorrhagia.
Risk factors
Risk factors vary with age and whether you have other medical conditions that may describe your menorrhagia. In a normal cycle, the release of an egg from the ovaries promotes the body’s production of progesterone, the female hormone most responsible for keeping durations regular. When no egg is launched, inadequate progesterone can cause heavy menstrual bleeding.
Menorrhagia in adolescent girls is usually due to anovulation. Adolescent girls are particularly prone to anovulatory cycles in the first year after their first menstrual period (menarche).
Menorrhagia in older reproductive-age women is usually due to uterine pathology, including fibroids, polyps and adenomyosis. However, other issues, such as uterine cancer, bleeding conditions, medication side effects and liver or kidney disease need to be eliminated.
Does Heavy Menstrual Bleeding With Clots Dangerous?
Extreme or extended menstrual bleeding can cause other medical conditions, consisting of:
Anemia. Menorrhagia can cause blood loss anemia by lowering the variety of circulating red cell. The variety of distributing red blood cells is determined by hemoglobin, a protein that makes it possible for red cell to bring oxygen to tissues.
Iron deficiency anemia takes place as your body tries to make up for the lost red blood cells by using your iron stores to make more hemoglobin, which can then carry oxygen on red blood cells. Menorrhagia might decrease iron levels enough to increase the risk of iron deficiency anemia.
Symptoms and signs consist of pale skin, weak point and tiredness. Although diet plays a role in iron deficiency anemia, the problem is complicated by heavy menstrual periods.
Severe pain. Along with heavy menstrual bleeding, you might have painful menstrual cramps (dysmenorrhea). Sometimes the cramps associated with menorrhagia are severe enough to need medical examination.
Treatment
Particular treatment for menorrhagia is based on a variety of elements, including:
- Your future childbearing plans
- The cause and intensity of the condition
- Your tolerance for particular medications, treatments or therapies
- Your opinion or individual preference
- Impacts of the condition on your lifestyle
- The likelihood that your periods will end up being less heavy quickly
- Your overall health and case history
Used Medications
Medical therapy for menorrhagia might include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs, such as ibuprofen (Advil, Motrin IB, others) or naproxen salt (Aleve), help in reducing menstrual blood loss. NSAIDs have the included advantage of relieving painful menstrual cramps (dysmenorrhea).
- Tranexamic acid. Tranexamic acid (Lysteda) helps reduce menstrual blood loss and only has to be taken at the time of the bleeding.
- Oral contraceptives. Aside from supplying contraception, contraceptive pills can assist manage menstrual cycles and decrease episodes of extreme or prolonged menstrual bleeding.
- Oral progesterone. The hormone progesterone can help fix hormone imbalance and reduce menorrhagia.
- Hormonal IUD (Liletta, Mirena). This intrauterine device releases a kind of progestin called levonorgestrel, that makes the uterine lining thin and reduces menstrual blood circulation and cramping.
If you have menorrhagia from taking hormone medication, you and your doctor may be able to treat the condition by changing or stopping your medication.
If you likewise have anemia due to your menorrhagia, your doctor may suggest that you take iron supplements routinely. If your iron levels are low but you’re not yet anemic, you might be begun on iron supplements instead of waiting till you become anemic.
Procedures to Follow
You might need surgical treatment for menorrhagia if medical therapy is unsuccessful. Treatment alternatives include:
- Dilation and curettage (D&C). In this procedure, your doctor opens (dilates) your cervix then scrapes or suctions tissue from the lining of your uterus to reduce menstrual bleeding. Although this procedure is common and frequently treats acute or active bleeding effectively, you might require additional D&C treatments if menorrhagia repeats.
- Uterine artery embolization. For women whose menorrhagia is caused by fibroids, the goal of this procedure is to shrink any fibroids in the uterus by obstructing the uterine arteries and cutting off their blood supply. During uterine artery embolization, the surgeon passes a catheter through the big artery in the thigh (femoral artery) and guides it to your uterine arteries, where the blood vessel is injected with products that decrease blood flow to the fibroid.
- Focused ultrasound surgery. Just like uterine artery embolization, focused ultrasound surgery deals with bleeding brought on by fibroids by shrinking the fibroids. This procedure uses ultrasound waves to damage the fibroid tissue. There are no incisions needed for this procedure.
- Myomectomy. This procedure includes surgical elimination of uterine fibroids. Depending on the size, number and place of the fibroids, your surgeon might choose to carry out the myomectomy using open abdominal surgery, through several little cuts (laparoscopically), or through the vaginal area and cervix (hysteroscopically).
- Endometrial ablation. This procedure includes damaging (ablating) the lining of your uterus (endometrium). The procedure uses a laser, radiofrequency or heat used to the endometrium to ruin the tissue.
- After endometrial ablation, the majority of women have much lighter periods. Pregnancy after endometrial ablation has actually many associated complications. If you have endometrial ablation, using reputable or long-term birth control till menopause is recommended.
- Endometrial resection. This surgery uses an electrosurgical wire loop to remove the lining of the uterus. Both endometrial ablation and endometrial resection advantage women who have extremely heavy menstrual bleeding. Pregnancy isn’t suggested after this procedure.
- Hysterectomy. Hysterectomy — surgery to remove your uterus and cervix — is a long-term procedure that causes sterility and ends menstrual periods. Hysterectomy is carried out under anesthesia and needs hospitalization. Extra elimination of the ovaries (bilateral oophorectomy) may cause premature menopause.
A lot of these surgical procedures are done on an outpatient basis. Although you might need a basic anesthetic, it’s most likely that you can go home later on the very same day. An abdominal myomectomy or a hysterectomy usually requires a health center stay.
When menorrhagia signifies another condition, such as thyroid disease, treating that condition typically results in lighter durations.