What is idiopathic intracranial hypertension?
Intracranial hypertension is a condition due to high pressure within the spaces that surround the brain and spinal cord. These spaces are filled with cerebrospinal fluid (CSF), which cushions the brain from mechanical injury, provides nutrition, and carries away waste.
The most typical symptoms of intracranial hypertension are headaches and visual loss, including blind spots, poor peripheral (side) vision, double vision, and short temporary episodes of blindness. Many patients experience permanent vision loss. Other common symptoms consist of pulsatile tinnitus (ringing in the ears) and neck and shoulder pain.
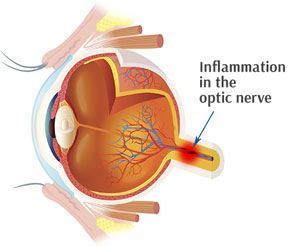
Intracranial hypertension can be either acute or persistent. In persistent intracranial hypertension, the increased CSF pressure can trigger swelling and damage to the optic nerve– a condition called papilledema.
Chronic intracranial hypertension can be caused by many conditions consisting of certain drugs such as tetracycline, an embolism in the brain, excessive consumption of vitamin A, or brain growth. It can also occur without a noticeable cause. This is idiopathic intracranial hypertension (IIH).
Due to the fact that the symptoms of IIH can look like those of a brain growth, it is sometimes known by the older name pseudotumor cerebri, which suggests “incorrect brain tumor.”
Signs and Symptoms of Idiopathic Intracranial Hypertension
The most typical symptom of IIH is headache, which takes place in practically all (92– 94 %) cases. It is typically even worse in the early morning, generalized in character and throbbing in nature. It may be connected with queasiness and throwing up. The headache can be made worse by any activity that further enhances the intracranial pressure, such as coughing and sneezing. The pain may likewise be experienced in the neck and shoulders. Numerous have pulsatile tinnitus, a whooshing experience in one or both ears (64– 87 %); this noise is concurrent with the pulse. Various other symptoms, such as numbness of the extremities, generalized weakness, loss of smell, and loss of coordination, are reported more seldom; none are certain for IIH. In children, many nonspecific symptoms and signs might be present.
The increased pressure results in compression and traction of the cranial nerves, a group of nerves that arise from the brain stem and provide the face and neck. The majority of typically, the abducens nerve (sixth nerve) is included. This nerve provides the muscle that pulls the eye external. Those with sixth nerve palsy therefore experience horizontal double vision which is worse when looking to the affected side. More seldom, the oculomotor nerve and trochlear nerve (third and fourth nerve palsy, respectively) are influenced; both play a role in eye motions. The facial nerve (7th cranial nerve) is influenced occasionally – the outcome is total or partial weak point of the muscles of facial expression on one or both sides of the face.
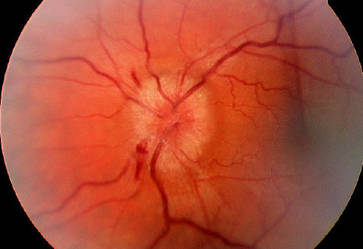
The increased pressure causes papilledema, which is swelling of the optic disc, the spot where the optic nerve enters the eyeball. This takes place in almost all cases of IIH, however not everybody experiences symptoms from this. Those who do experience symptoms typically report “short-term visual obscurations”, episodes of trouble seeing that occur in both eyes but not always at the exact same time. Long-term unattended papilledema leads to visual loss, at first in the periphery but gradually towards the center of vision.
Physical exam of the worried system is usually typical apart from the presence of papilledema, which is seen on evaluation of the eye with a little device called an ophthalmoscope or in more information with a fundus video camera. If there are cranial nerve irregularities, these might be observed on eye examination in the form of a squint (third, fourth, or sixth nerve palsy) or as facial nerve palsy. If the papilledema has been longstanding, visual fields may be constricted and visual acuity may be reduced. Visual field testing by automated (Humphrey) perimetry is advised as other approaches of testing might be less precise. Longstanding papilledema causes optic atrophy, in which the disc looks light and visual loss tends to be advanced.
Who is at risk for IIH?
An approximated 100,000 Americans have IIH, and the number is rising as more individuals end up being overweight or obese. The condition is most common in females between the ages of 20 and 50; about 5 percent of those affected are men. Obesity, defined as a body mass index (BMI) greater than 30, is a major risk element. BMI is a number based on your weight and height. The Centers for Disease Control and Prevention provides an online BMI calculator. A current gain of 5-15 percent of total body weight is likewise considered a danger factor for this condition, even for people with a BMI less than 30.
How is IIH diagnosed?
A thorough case history and physical exam are had to recognize threat elements for IIH and to assess for the lots of possible reasons for enhanced intracranial pressure. A neurological test will likewise be carried out. In IIH, the exam is normal except for findings related to enhanced intracranial pressure, including papilledema, visual loss, and possible weak point in the lateral rectus muscles, which are located near your temples and help turn the eyes outside. Weak point in these muscles can trigger the eyes to turn inward, towards the nose, producing double vision.
A number of vision tests may also be performed, consisting of a detailed dilated eye exam to search for signs of papilledema. Visual field screening is done to examine your peripheral vision. This screening measures the area of area you can see at a provided instant without moving your head or eyes.
Brain imaging, consisting of computed tomography (CT) and magnetic resonance imaging (MRI) scans, will be carried out to try to find a brain growth, injury, or other prospective cause for your symptoms. Regular findings on these tests are essential to a diagnosis of IIH.
A lumbar leak, also referred to as a spine tap, will be performed. In this procedure, a needle is inserted into a CSF-filled sac listed below the spinal cord in the lower back. The CSF pressure will be measured, and a percentage of CSF will be collected for analysis to look for causes of enhanced intracranial pressure. The treatment might likewise trigger a temporary reduction in CSF pressure and symptoms.
IIH Treatment
If a medical diagnosis of IIH is confirmed, routine visual field tests and thorough dilated eye tests are recommended to keep an eye on any changes in vision.
Sustainable weight loss through healthy consuming, salt restriction, and workout is a crucial part of treatment for individuals with IIH who are obese. Research studies reveal that modest weight reduction, around 5-10 percent of total body weight, may be sufficient to reduce signs and symptoms. If way of life modifications are not successful in minimizing weight and relieving IIH, weight reduction surgery might be recommended for those with a BMI higher than 40.
For many individuals, weight loss can be difficult to attain and keep. And for those who are able to change their weight, relief from IIH tends to be progressive. Acetazolamide (Diamox), a drug that decreases CSF production, is therefore frequently made use of as an add-on treatment to weight loss. The drug is taken orally. Typical side effects consist of tiredness, queasiness, tingling hands and feet, and a metallic taste, generally activated by soft drinks. These can be reversed by lowering the dose or stopping the drug.
It’s crucial to keep in mind that some medications, such as tetracycline, might assist trigger IIH, which stopping them might lead to improvement.
In quickly progressive cases that do not react to other treatments, surgery might be needed to alleviate pressure on the optic nerve. Healing shunting, which includes surgically placing a tube to drain CSF from ventricles or inner brain cavities, can be utilized to remove excess CSF and lower pressure. In a treatment called optic nerve sheath fenestration, pressure on the optic nerve is relieved by making a small window into the covering that surrounds the nerve just behind the eyeball.
What is the diagnosis?
For the majority of people, IIH generally enhances with treatment. For others, it gradually aggravates with time, or it can resolve and then recur. About 5-10 percent of ladies with IIH experience disabling vision loss. The majority of patients do not need medical treatment.
What research study is being done?
For years, acetazolamide has actually been the drug of choice for treating IIH, however with little proof that it helped and no recognized usage standards. The NEI-funded IIH Treatment Trial was designed to investigate the benefits of acetazolamide for IIH in patients with mild visual loss, and balance them against the drug’s known side effects. The trial compared acetazolamide plus a weight reduction plan, versus the same weight reduction plan with a placebo tablet, among 161 women and 4 men who had mild vision loss from IIH. To restrict side effects, the dose was slowly increased to a maximally endured dose or as much as 4 grams daily. In 2014, the scientists reported that the drug– weight reduction combination helped to preserve as well as restore vision over a six-month period. The trial will continue for a total of five years.
There is also continuous research study to identify what causes IIH. There have been some reports of IIH in numerous generations within households, suggesting that genes may contribute. Because of its relationship to gender and obesity, there is a strong possibility that hormonal agents add to IIH. Some hormonal agents are really released from fat, and are being studied as possible consider the disease. The IIH Treatment Trial includes procedures to deal with the role of genetics and hormonal agents in IIH.