Medullary thyroid cancer (also known as medulla thyroid cancer) is the 3rd most typical type of thyroid cancer. This short article will discuss common medullary thyroid cancer symptoms and treatments in addition to medullary thyroid cancer medical diagnosis and diagnosis.
Medullary tumors are the 3rd most common of all thyroid cancers. They make up about 3% of all thyroid cancer cases.
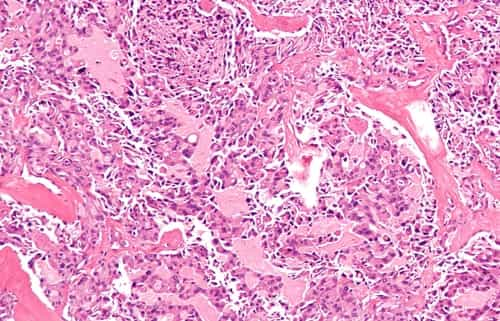
However what are some common medullary thyroid cancer symptoms? Unlike papillary thyroid cancer and follicular thyroid cancer that emerge from thyroid hormone producing cells, medullary thyroid cancer originates from the parafollicular cells (also called C cells) of the thyroid.
These C cells make a various hormone called calcitonin, which has nothing to do with the control of metabolic process the way thyroid hormone does. As you will see below, the production of this hormone can be measured after an operation to determine if the cancer is still present and if it is growing.
Symptoms and Signs
The significant medical symptom of metastatic medullary thyroid cancer is diarrhea; sometimes a patient will have flushing episodes. Both take place especially with liver metastasis, and either symptom might be the first symptom of the disease. The flushing that happens in medullary thyroid carcinoma is identical from that connected with carcinoid syndrome. In MTC, the flushing, diarrhea, and itching (pruritis) are all triggered by raised levels of calcitonin gene products (calcitonin or calcitonin gene-related peptide). Additionally, the flushing and diarrhea observed in carcinoid syndrome is brought on by raised levels of flowing serotonin.
Medullary thyroid carcinoma may likewise produce a thyroid blemish and bigger cervical lymph nodes.
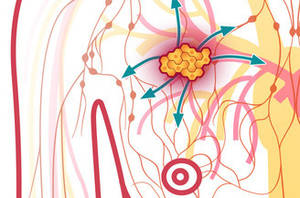
Sites of spread of medullary thyroid cancer include local lymph nodes in the neck, lymph nodes in the central part of the chest (mediastinum), liver, lung, and bone. Spread to other sites such as skin or brain happens but is unusual.
Medullary Thyroid Cancer Facts
- Happens in 4 medical settings (see below) and can be associated with other endocrine tumors
- Recurring disease (following surgery) or recurrence can be found by determining calcitonin (a hormone that ought to be measured every 4 months for the first couple of years then every 6 months for the rest of your life).
- Regional metastases (spread to neck lymph nodes) occurs early in the disease.
- Not related to radiation direct exposure.
- Typically originates in the upper central lobe of the thyroid.
- More common in females than males (except for acquired cancers).
- Infect far-off organs (metastasis) takes place late and can be to the liver, bone, brain, and adrenal medulla.
- Poor prognostic elements consist of mean older than 50 years old, far-off spread (metastases), when seen in patients with other endocrine tumors due to MEN II-B syndrome.
4 Types Of the Cancer
- Sporadic: Accounts for 80% of all cases of medullary thyroid cancer. They are generally unilateral and there are not associated endocrinopathies (not connected with disease in other endocrine glands). Peak onset is in between 40 and 60 years of ages. Females out number males by a 3:2 ratio. One 3rd will provide with intractable diarrhea. Diarrhea is caused by increased intestinal secretion and hypermotility due to the hormonal agents produced by the tumor (calcitonin, prostaglandins, serotonin, or VIP).
- MEN II-A (Sipple Syndrome): Multiple endocrine neoplasia syndromes (abbreviated as “MEN”) are a group of endocrine disorders that happen together in the very same patient and normally are seen in households since they are acquired. “Syndromes” are medical conditions that happen in groups of 3.
- Sipple syndrome has 1) bilateral medullary cancer or C cell hyperplasia, 2) pheochromocytoma, and 3) hyperparathyroidism.
- This syndrome is acquired and is because of a flaw of a gene (DNA) that helps control the normal growth of endocrine tissues. This acquired syndrome is passed on to all children who get the gene (inherited in an autosomal dominant fashion), which theoretically, would be 50% of all offspring of a person with this defective gene. Since of this, males and women are similarly affected. Peak occurrence of medullary carcinoma in these patients remains in the 30s.
- MEN II-B. With this syndrome, patients might likewise have 1) medullary carcinoma and 2) pheochromocytoma, however only rarely will they have hyperparathyroidism. Rather these patients have 3) an uncommon look that is identified by mucosal ganglioneuromas (tumors in the mouth) and a Marfanoid habitus.
- Inheritance is autosomal dominant as in MEN II-A, or it can take place sporadically (without being inherited). MEN II-B patients normally get medullary cancer in their 30s, and males and women are similarly effected. Similar To MEN II-A, pheochromocytomas should be found prior to any operation. The idea here is to remove the pheochromocytoma first to remove the risk of severe hypertensive episodes while the thyroid or parathyroid is being run on.
- Inherited medullary carcinoma without associated endocrinopathies. This kind of medullary cancer is the least aggressive. Similar to other types of thyroid cancers, the peak incidence is in between 40 and 50 years old.
How Is Medullary Thyroid Cancer Treated
Thyroid gland has actually 2 lobes linked by an isthmus. In contrast to papillary and follicular cancers, little debate exits when discussing how to treat medullary thyroid cancer. After assessment and treatment of associated endocrine conditions (such as pheochromocytomas if present) by an endocrinologist, all patients need to receive total thyroidectomy, a total main neck dissection (elimination of all lymph nodes and fats in the main area of the neck), and elimination of all lymph nodes and surrounding fatty tissues within the side of the neck where the tumor was present.
A diagram of thyroid operations are covered in greater detail (with illustrations) in our post about the numerous thyroid surgery options.
Radioactive Iodine
Although thyroid cells have the cellular system to soak up iodine, medullary thyroid cancer does not emerge from this kind of thyroid cell. Therefore, radioactive iodine therapy is not helpful for the treatment of medullary thyroid cancer. Similarly, if medullary cancer spreads to remote sites, it can not be found by iodine scanning the manner in which far-off spread from papillary or follicular cancer can.
How to Live With Medullary Thyroid Cancer?
In addition to the normal cancer follow up, patients must get a yearly chest x-ray in addition to calcitonin levels. Serum calcitonin is extremely useful in follow up of medullary thyroid cancer because no other cells of the body make this hormone. A high serum calcitonin level that had actually formerly been low following total thyroidectomy is indicative of recurrence.
Under the best situations, thyroid surgery will remove all of the thyroid and all lymph nodes in the neck that harbor metastatic spread. In this case, post-operative calcitonin levels will go to absolutely no. This is often not the case, and calcitonin levels remain raised, but less than pre-operatively. These levels should still be inspected every 6 months, and when they start to increase, a more diligent evaluation remains in order to find the source.
What Is the Survival Rate for Medullary Thyroid Cancer?
This cancer has a much lower cure rate than does the well-differentiated thyroid cancers (papillary and follicular), but treatment rates are higher than they are for anaplastic thyroid cancer. In general, 10-year survival rates are 90% when all the disease is restricted to the thyroid gland; 70% with infect cervical lymph nodes; and 20% when spread to far-off sites.
Overall, the prognosis for patients with medullary thyroid cancer is good. The 10-year survival rate for patients with medullary thyroid cancer is 75%-85%. Roughly half of the patients with medullary thyroid cancer present with disease localized to the thyroid gland, and these patients have a 10-year survival rate of 95.6%. One third of patients present with in your area invasive tumors or medically apparent infect the local lymph nodes. Patients with regional disease have a 5-year general survival rate of 75.5%. Far-off metastases are present in 13% of patients at preliminary diagnosis and hint a bad diagnosis, with a 10-year survival rate of just 40%.
Conclusion
There are numerous treatment choices for medullary thyroid cancer, including external beam radiation and a thyroidectomy. Speak to your doctor about which treatment options are right for you.