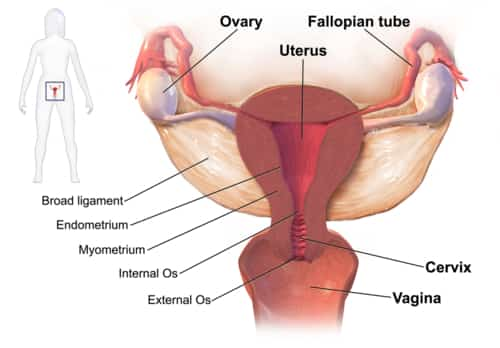
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs. It generally happens when sexually transmitted bacteria spread out from your vaginal area to your uterus, fallopian tubes or ovaries.
Pelvic inflammatory disease frequently causes no signs or symptoms. As an outcome, you might not realize you have the condition and get required treatment. The condition may be spotted later on if you have trouble getting pregnant or if you develop chronic pelvic pain.
Symptoms of Pelvic Inflammatory Disease
Symptoms and signs of pelvic inflammatory disease may consist of:
- Pain in your lower abdominal area and pelvis
- Heavy vaginal discharge with an undesirable smell
- Irregular uterine bleeding, particularly during or after intercourse, or between menstrual cycles
- Pain or bleeding during intercourse
- Fever, in some cases with chills
- Painful or difficult urination
PID might cause just mild symptoms and signs or none at all. When severe, PID may cause fever, chills, severe lower abdominal or pelvic pain– specifically during a pelvic exam — and bowel pain.
When to see a doctor
See your doctor or look for urgent medical care if you experience:
- Severe pain low in your abdomen
- Nausea and vomiting, with a failure to keep anything down
- Fever, with a temperature higher than 101 F (38.3 C).
- Foul vaginal discharge.
If your signs and symptoms continue but aren’t severe, see your doctor as quickly as possible. Vaginal discharge with a smell, painful urination or bleeding in between menstruations can be related to a sexually transmitted infection (STI). If these symptoms and signs take place, stop having sex and see your doctor quickly. Prompt treatment of an STI can help prevent PID.
Causes of Pelvic Inflammatory Disease
Numerous types of bacteria can cause PID, but gonorrhea or chlamydia infections are the most common. These bacteria are generally acquired during unguarded sex.
Less typically, bacteria can enter your reproductive tract anytime the normal barrier developed by the cervix is interrupted. This can occur after childbirth, miscarriage or abortion.
Risk factors
A number of elements may increase your risk of pelvic inflammatory disease, including:
- Being a sexually active woman younger than 25 years of ages.
- Having multiple sexual partners.
- Remaining in a sexual relationship with a person who has more than one sex partner.
- Making love without a prophylactic.
- Douching regularly, which upsets the balance of good versus harmful bacteria in the vagina and may mask symptoms.
Having a history of pelvic inflammatory disease or a sexually transmitted infection. Most professionals now concur that having an intrauterine device (IUD) inserted does not increase the risk of pelvic inflammatory disease. Any prospective risk is generally within the first three weeks after insertion.
Complications
Unattended pelvic inflammatory disease might cause scar tissue. You might likewise establish collections of infected fluid (abscesses) in your fallopian tubes, which could harm your reproductive organs.
Other complications might consist of:
- Ectopic pregnancy. PID is a significant reason for tubal (ectopic) pregnancy. In an ectopic pregnancy, the scar tissue from PID avoids the fertilized egg from making its way through the fallopian tube to implant in the uterus. Ectopic pregnancies can cause huge, dangerous bleeding and need emergency situation medical attention.
- Infertility. PID may damage your reproductive organs and cause infertility– the inability to become pregnant. The more times you’ve had PID, the greater your risk of infertility. Postponing treatment for PID likewise significantly increases your risk of infertility.
- Chronic pelvic pain. Pelvic inflammatory disease can cause pelvic pain that might last for months or years. Scarring in your fallopian tubes and other pelvic organs can cause pain during sexual intercourse and ovulation.
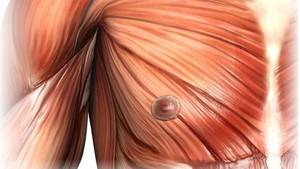
- Tubo-ovarian abscess. PID might cause an abscess– a collection of pus– to form in your uterine tube and ovaries. If left without treatment, you might establish a dangerous infection.
Prevention for Pelvic Inflammatory Disease
To reduce your risk of pelvic inflammatory disease:
- Talk with your doctor about contraception. Lots of kinds of contraception do not safeguard versus the advancement of PID. Using barrier techniques, such as a prophylactic, may assist to decrease your risk. Even if you take birth control pills, it’s still essential to use a prophylactic each time you have sex to protect against STIs.
- Get evaluated. If you’re at risk of an STI, such as chlamydia, make a consultation with your doctor for screening. Establish a regular screening schedule with your doctor if needed. Early treatment of an STI gives you the best chance of preventing PID.
- Request that your partner be checked. If you have pelvic inflammatory disease or an STI, encourage your partner to be checked and, if required, dealt with. This can prevent the spread of STIs and possible reoccurrence of PID.
- Don’t douche. Douching upsets the balance of bacteria in your vagina.
Diagnosis
Medical professionals detect pelvic inflammatory disease based on symptoms and signs, a pelvic examination, an analysis of vaginal discharge and cervical cultures, or urine tests.
During the pelvic test, your doctor will first check your pelvic region for signs and symptoms of PID. Your doctor may then use cotton bud to take samples from your vaginal area and cervix. The samples will be examined at a laboratory to figure out the organism that’s triggering the infection.
To verify the medical diagnosis or to figure out how extensive the infection is, your doctor might advise other tests, such as:.
- Blood and urine tests. These tests will determine your white blood cell count, which may show an infection, and markers that recommend inflammation. Your doctor also might advise tests for HIV and sexually sent infections, which are often related to PID.
- Ultrasound. This test uses sound waves to produce images of your reproductive organs.
- Laparoscopy. During this procedure, your doctor inserts a thin, lighted instrument through a little cut in your abdomen to view your pelvic organs.
Treatment for Pelvic Inflammatory Disease
Treatments for pelvic inflammatory disease include:
- Antibiotics. Your doctor will recommend a combination of antibiotics to start right away. After getting your laboratory test results, your doctor might adjust your prescription to much better match what’s triggering the infection. You will likely subsequent with your doctor after three days to make sure the treatment is working.Make sure to take all your medication, even if you start to feel better after a couple of days. Antibiotic treatment can help prevent major complications however can’t reverse any damage.
- Treatment for your husband. To prevent reinfection with an STI, your husband ought to be examined and treated. Infected husband may not have any visible symptoms.
- Temporary abstaining. Prevent sexual relations until treatment is finished and tests show that the infection has cleared in all partners.
The majority of women with pelvic inflammatory disease simply require outpatient treatment. Nevertheless, if you’re seriously ill, pregnant or haven’t responded to oral medications, you might require hospitalization. You might get intravenous antibiotics, followed by antibiotics you take by mouth.
Surgery is seldom necessary. Nevertheless, if an abscess ruptures or threatens to burst, your doctor may drain it. You also may need surgery if you don’t respond to antibiotic treatment or have a questionable diagnosis, such as when one or more of the signs or symptoms of PID are absent.
Coping and support
Lots of women are diagnosed with PID together with a sexually transmitted infection. Learning that you have an STI can be distressing. Take actions right away to get dealt with and to prevent reinfection.
If you’ve experienced more than one episode of pelvic inflammatory disease, you’re at higher risk of infertility. If you’ve been attempting to conceive without success, make an appointment with your doctor for an infertility examination.
Your doctor or a reproductive health professional may do tests to figure out whether or not your history of pelvic inflammatory disease is triggering the issue.
Getting ready for your appointment
If you have signs or symptoms of pelvic inflammatory disease, make a consultation to see your doctor or other healthcare service provider.
Here’s some information on what you can do to get ready and what to get out of your doctor.
What you can do
- Know any pre-appointment limitations. At the time you make the appointment, ask if there’s anything you have to perform in advance.
- Write down any symptoms you’re experiencing, consisting of any that might seem unrelated to the reason for which you set up the appointment.
- Make a list of all medications, vitamins or supplements that you’re taking.
- Make a note of concerns to ask your doctor.
Some fundamental concerns to ask include:
What kinds of tests do I need?
Is this a sexually transmitted infection?
Should my partner be evaluated or dealt with?
Do I have to stop having sex during treatment? How long should I wait?
How can I prevent future episodes of pelvic inflammatory disease?
Will this affect my capability to end up being pregnant?
Exists a generic option to the medication you’re recommending me?
Can I be treated at home? Or will I have to go to a health center?
Do you have any printed products that I can take with me? What sites do you suggest?
Do I have to return for a follow-up see?
What to get out of your doctor
Your doctor is likely to ask you a number of concerns, such as:
Do you have a new sexual partner or multiple partners?
Do you always use prophylactics?
When did you first begin experiencing symptoms?
What are your symptoms?
Are you experiencing any pelvic pain?
How severe are your symptoms?