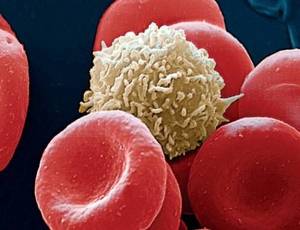
Balamuthia mandrillaris (B. mandrillaris) is an amoeba that resides in water and soil. B. mandrillaris was first found in 1990 and has actually been connected with more than 100 cases of disease since then. Infection with B. mandrillaris has actually been reported in South, Central, and North America, Asia, Australia, and Europe however stays a rare reason for amoebiasis.
Causes
B. mandrillaris can enter humans through the nasal mucosa, lungs, or breaks in the skin. As in cases of other free-living amoebae (e.g. Naegleria and Acanthamoeba), a history of swimming in freshwater lakes, ponds, and heated pool appears to be common.
Weeks to years later on (5 to 8 months usually) the infection spreads to the central nervous system triggering amoebic sleeping sickness (inflammation of the brain).
Symptoms Balamuthia Mandrillaris Encephalitis
Features of B. mandrillaris encephalitis include:
- fever
- focal neurological deficits (e.g. double vision has been frequently reported).
- symptoms of meningeal irritation (e.g. neck stiffness, intolerance to bright light).
- symptoms of increased intracranial pressure– e.g. headache, nausea and vomiting, reduced level of awareness.
In 95% of patients, B. mandrillaris sleeping sickness is deadly.
Balamuthia mandrillaris and Skin
The dermatological significance of B. mandrillaris is that a common skin sore appears prior to the infection infects the main nervous system. The classical skin sore is an asymptomatic granulomatous plaque (a nodule made of inflammatory cells), typically located on the central face. They are typically described as rubbery in consistency. Single or multiple sores may be present. The sore might enlarge (to include the entire face sometimes), and sometimes gives origin to smaller sized satellite sores. Ulceration takes place at a late stage. Sometimes the sore may occur on the extremities.
Diagnosis
As B. mandrillaris infection is very uncommon, diagnosis is frequently postponed. Medical diagnosis is made by discovering the amoeba in the skin or other tissue. Biopsy reveals tuberculoid granulomatous infiltrate within dermis and subcutaneous tissues. Trophozoites and cysts are seldom seen.
B. mandrillaris is tough to culture in the laboratory within normal culture media. The organism can be grown in specific mammalian cell culture lines or by innoculation of mice if there is scientific suspicion of balamuthia infection. A polymerase chain reaction (PCR) test has actually been established for research study functions however is not currently available in neighborhood laboratories.
Treatment of Balamuthia Mandrillaris Infection
Early treatment with a series of oral antifungal, anthelmintic, and antiprotozoal drugs (often in mix) may enhance survival. Balamuthia infection has had successful treatments.
Case study
In two cases, both were treated with a cocktail of antibiotics and antifungal drugs, although it is unclear if any or all of these medications played a part in treatment. Both victims suffered irreversible neurological deficits as an outcome of their infection.
Another two cases existed and both of these people received effective treatments due to discovering the infection early. Two people, a five-year-old lady and a 64-year-old man, developed GAE. After medical diagnosis, they were given effective antimicrobial therapy. Both patients recovered.
B. mandrillaris photo credit: uab.edu