Cardiac asthma is not a form of asthma. It’s a type of coughing or wheezing that occurs with left heart failure. Depending upon how extreme your signs and symptoms are, this hissing can be a medical emergency situation. Heart failure can create liquid to accumulate in your lungs (pulmonary edema) and in and around your airways. This can create shortness of breath, coughing and wheezing comparable to the signs and symptoms of asthma.
Real asthma is a chronic problem brought on by inflammation of the airways, which can tighten them, causing breathing problems. Real asthma has nothing to do with fluid in the lungs or heart disease.
The difference is necessary because treatments for asthma and heart failure are various. Treatments for heart failure can aid boost your signs of both heart failure and cardiac asthma. Overusing treatments for true asthma, such as rescue inhalers, could be dangerous and potentially result in a worsening of signs.
What are the Signs of Cardiac Asthma?
Symptoms of cardiac asthma consist of:
- wheezing
- difficulty breathing
- rapid breathing
- coughing
- groaning
- bloody spit
- frothy sputum
- orthopnea (lack of breath when relaxing).
- rales (abnormal noises heard when listening to the lung with a stethoscope).
- paroxysmal nighttime dyspnea (awakening during the night wheezing for air).
Symptoms of cardiac asthma may be the preliminary symptoms of heart failure, or they might be present in addition to various other indications of heart failure, such as:
- breast discomfort.
- fainting.
- tiredness.
- irregular heart price.
- skin that appears blue.
- swelling in the legs, feet, or ankle joints.
- weight gain from liquid retention.
- increased requirement to urinate, frequently in the evening.
How is it Diagnosed?
Cardiac asthma can be tough to identify due to its resemblance to asthma. Misdiagnosis prevails. To distinguish in between both, a physician will likely begin by taking a look at your case history and risk factors to determine whether heart failure is the reason.
Tests that might be executed to help detect heart failure include:
- Physical exam. The medical professional may search for various other indications of cardiac asthma and heart failure, such as uncommon noises in your lungs when breathing and uncommon heart price.
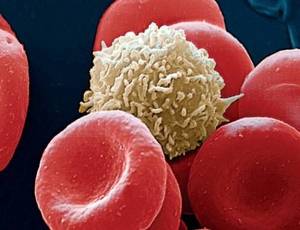
- Blood tests. The doctor might suggest a blood examination to aid diagnose problems that can lead to heart failure, check for markers of enhanced fluid, and dismiss various other potential reasons for your signs and symptoms.
- Electrocardiogram. An electrocardiogram checks the electrical activity of your heart and aids identify abnormalities in your heart rhythm.
- Echocardiogram. An echocardiogram is a type of ultrasound that utilizes acoustic waves to create a photo of your heart. The picture can show the physician just how much blood your heart is pumping and screen for abnormalities or abnormalities in the pumping feature.
- Chest X-ray. A chest X-ray can help identify an enlarged heart or fluid in your lungs.
- Breathing examinations. Your doctor might recommend breathing examinations like a spirometry test or a top flow test to display for lung issues.
- Other imaging methods. A CT or MRI scan may additionally be utilized to generate images to assess the wellness of your heart.
What Causes Cardiac Asthma?
Cardiac asthma is triggered by heart failure. The most usual root cause of heart failure in grownups is coronary artery disease. Coronary artery condition is when the arteries that provide blood to the heart end up being narrowed or blocked, unable to supply blood and even shutting completely because of a heart attack. It’s generally triggered by atherosclerosis, or the build-up of cholesterol and plaque in the blood vessels.
Other problems that can trigger or contribute to the development of heart failure consist of:
- previous cardiac arrest.
- abnormal heart rhythm.
- uncontrolled high blood pressure.
- heart shutoff conditions.
- cardiomyopathy.
- hyperthyroidism.
- myocarditis.
- heart defects existing from birth.
- diabetes.
- serious lung condition.
- excessive weight.
- kidney failing.
- severe anemia.
- rest apnea.
What are the Current Treatment Options?
Classic asthma medications like bronchodilators are thought to have restricted performance for dealing with cardiac asthma. Treatment for cardiac asthma involves addressing the hidden heart failure and fluid build-up in the lungs.
Medications
Medications commonly used to deal with an emergency situation case of cardiac asthma include:.
- morphine.
- furosemide or diuretics to get rid of fluid.
- nitroglycerin.
When your signs and symptoms maintain, you may be given ACE inhibitors or beta-blockers or both to prevent an additional episode. ACE inhibitors assist expand blood vessels and discharge the heart, while beta-blockers slow your heart rate and lower your blood pressure.
Oxygen and Ventilation
If your body isn’t getting enough oxygen, you’ll likely be provided oxygen or place on a noninvasive ventilator. In serious situations, you could require a breathing tube. Nonetheless, these treatments aren’t essential if you’re able to breathe well enough to get appropriate oxygen.
Surgery
Some people will certainly need surgical interventions, such as an angioplasty or coronary bypass surgery, to enhance blood circulation to the heart and make the heart more powerful. The final therapy option when all other therapies have stopped working is a heart transplant.
What’s the Outlook for People With Cardiac Asthma?
Cardiac asthma is a secondary condition triggered by heart failure. The outlook for people with heart failure boosts the earlier they get proper treatment. Nevertheless, it can vary extensively between people.
The life span of someone with cardiac asthma depends upon how far their heart failure has advanced, the underlying cause, and their total health.
Mortality rates at 1 year and 5 years after heart failure diagnosis are about 22 and 43 percent, respectively.
The Bottom Line
Cardiac asthma is a condition brought on by heart failure that causes asthma-like signs and symptoms, such as wheezing, coughing, and difficulty breathing. It’s triggered by a build-up of fluid in the lungs due to the failure of the heart to effectively clear fluid from the lungs.
Cardiac asthma is often misdiagnosed as asthma, however a correct diagnosis is important for obtaining proper therapy maximizing your outlook.