Tests and diagnosis
Diagnosis of GERD is based upon:
- Your symptoms. Your doctor may have the ability to diagnose GERD based upon frequent heartburn and other symptoms.
- A test to monitor the amount of acid in your esophagus. Ambulatory acid (pH) probe tests use a device to determine acid for 24 hours. The device determines when, and for the length of time, stomach acid regurgitates into your esophagus. One type of screen is a thin, versatile tube (catheter) that’s threaded through your nose into your esophagus. The tube links to a small computer system that you use around your waist or with a strap over your shoulder.
Another type is a clip that’s put in your esophagus during endoscopy. The probe transmits a signal, also to a small computer system that you wear. After about two days, the probe falls off to be passed in your stool. Your doctor may ask that you stop taking GERD medications to get ready for this test.
If you have GERD and you’re a candidate for surgery, you may also have other tests, such as:
- An X-ray of your upper digestive system. Often called a barium swallow or upper GI series, this procedure involves drinking a milky liquid that coats and fills the within lining of your digestive tract. Then X-rays are taken of your upper digestive tract. The coating allows your doctor to see a shape of your esophagus, stomach and upper intestine (duodenum).
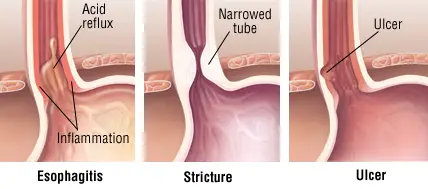
- A flexible tube to look inside your esophagus. Endoscopy is a way to visually analyze the inside of your esophagus and stomach. During endoscopy, your doctor inserts a thin, versatile tube geared up with a light and video camera (endoscope) down your throat, according to iytmed.com. Your doctor might likewise use endoscopy to collect a sample of tissue (biopsy) for additional screening. Endoscopy works in trying to find complications of reflux, such as Barrett’s esophagus.
- A test to measure the movement of the esophagus. Esophageal motility screening (manometry) measures movement and pressure in the esophagus. The test involves positioning a catheter through your nose and into your esophagus.
How Gastroesophageal reflux disease (GERD) Treated
Treatment for heartburn and other signs and symptoms of GERD usually starts with non-prescription medications that manage acid. If you do not experience relief within a few weeks, your doctor may recommend other treatments, consisting of medications and surgery.
Initial treatments to manage heartburn
Over-the-counter treatments that may help manage heartburn include:
- Antacids that neutralize stomach acid. Antacids, such as Maalox, Mylanta, Gelusil, Gaviscon, Rolaids and Tums, may provide fast relief. However antacids alone won’t heal an irritated esophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhea or constipation.
- Medications to reduce acid production. Called H-2-receptor blockers, these medications include cimetidine (Tagamet HB), famotidine (Pepcid Air Conditioning), nizatidine (Axid AR) or ranitidine (Zantac). H-2-receptor blockers don’t serve as quickly as antacids do, however they offer longer relief and may reduce acid production from the stomach for approximately 12 hours. More powerful variations of these medications are offered in prescription form.
- Medications that block acid production and heal the esophagus. Proton pump inhibitors are more powerful blockers of acid production than are H-2-receptor blockers and permit time for harmed esophageal tissue to heal.
- Over-the-counter proton pump inhibitors include lansoprazole (Prevacid 24 HR) and omeprazole (Prilosec, Zegerid OTC).
- Contact your doctor if you need to take these medications for longer than 2 to 3 weeks or your symptoms are not alleviated.
Prescription-strength medications
If heartburn persists regardless of initial approaches, your doctor may suggest prescription-strength medications, such as:
- Prescription-strength H-2-receptor blockers. These include prescription-strength cimetidine (Tagamet), famotidine (Pepcid), nizatidine (Axid) and ranitidine (Zantac).
- Prescription-strength proton pump inhibitors. Prescription-strength proton pump inhibitors include esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec, Zegerid), pantoprazole (Protonix), rabeprazole (Aciphex) and dexlansoprazole (Dexilant).
These medications are normally well-tolerated, but long-lasting use may be related to a minor increase in risk of bone fracture and vitamin B-12 shortage.
Medications to strengthen the lower esophageal sphincter. Baclofen may reduce the frequency of relaxations of the lower esophageal sphincter and for that reason decrease gastroesophageal reflux. It has less of an effect than do proton pump inhibitors, but it might be used in severe reflux disease. Baclofen can be associated with substantial side effects, the majority of commonly tiredness or confusion.
GERD medications are often combined to increase effectiveness.
Surgery and other treatments used if medications do not help.
Many GERD can be controlled through medications. In circumstances where medications aren’t valuable or you want to prevent long-term medication use, your doctor may recommend more-invasive treatments, such as:
- Surgery to strengthen the lower esophageal sphincter (Nissen fundoplication). This surgery includes tightening up the lower esophageal sphincter to prevent reflux by wrapping the very leading of the stomach around the outside of the lower esophagus. Surgeons usually perform this surgery laparoscopically. In laparoscopic surgery, the surgeon makes 3 or four small incisions in the abdomen and inserts instruments, including a versatile tube with a tiny cam, through the cuts.
- Surgery to reinforce the lower esophageal sphincter (Linx). The Linx device is a ring of tiny magnetic titanium beads that is twisted around the junction of the stomach and esophagus. The magnetic attraction in between the beads is strong enough to keep the opening between the two closed to refluxing acid, however weak enough so that food can travel through it. It can be implanted using minimally invasive surgery methods. This more recent device has been approved by the Food and Drug Administration and early studies with it appear promising.
Lifestyle and home remedies
Lifestyle changes might help reduce the frequency of heartburn. Consider aiming to:
- Preserve a healthy weight. Excess pounds put pressure on your abdominal area, pushing up your stomach and triggering acid to support into your esophagus. If your weight is healthy, work to keep it. If you are overweight or obese, work to slowly lose weight– no greater than 1 or 2 pounds (0.5 to 1 kg) a week. Ask your doctor for help in designing a weight-loss method that will work for you.
- Prevent tight-fitting clothing. Clothing that fit tightly around your waist put pressure on your abdomen and the lower esophageal sphincter.
- Avoid foods and beverages that set off heartburn. Everybody has specific triggers. Typical triggers such as fatty or fried foods, tomato sauce, alcohol, chocolate, mint, garlic, onion, and caffeine may make heartburn even worse. Prevent foods you understand will activate your heartburn. Quit drinking alcohol and smoking forever!
- Eat smaller meals. Prevent overindulging by eating smaller sized meals.
- Do not lie down after a meal. Wait at least 3 hours after eating before lying down or going to sleep.
- Raise the head of your bed. If you frequently experience heartburn at night or while attempting to sleep, put gravity to work for you. Place wood or cement blocks under the feet of your bed so that the head end is raised by 6 to 9 inches. If it’s not possible to raise your bed, you can place a wedge between your mattress and box spring to elevate your body from the waist up. Wedges are offered at drugstores and medical supply stores. Raising your head with extra pillows is ineffective.
- Don’t smoke. Cigarette smoking decreases the lower esophageal sphincter’s ability to operate properly.
Natural medicine
No option medicine therapies have been proved to treat GERD or to reverse damage to the esophagus. Still, some complementary and alternative therapies may provide some relief, when combined with your doctor’s care.
Speak with your doctor about what alternative GERD treatments may be safe for you.
- Herbal remedies. Herbal remedies in some cases used for GERD symptoms include licorice, slippery elm, chamomile, marshmallow and others. Herbal remedies can have serious side effects, and they might interfere with medications. Ask your doctor about a safe dosage prior to beginning any herbal remedy.








