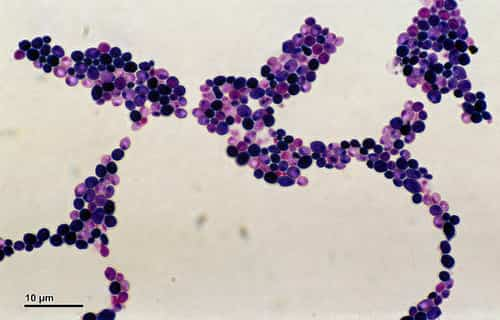
Candidiasis is infection by Candida sp (usually C. albicans), manifested by mucocutaneous lesions, fungemia, and often focal infection of multiple sites. Symptoms depend upon the site of infection and consist of dysphagia, skin and mucosal sores, blindness, vaginal symptoms (itching, burning, discharge), fever, shock, oliguria, renal shutdown, and distributed intravascular coagulation. Diagnosis is validated by histopathology and cultures from generally sterilized sites. Treatment is with amphotericin B, fluconazole, echinocandins, voriconazole, or posaconazole.
Meaning
Candida albicans sp are commensal organisms that inhabit the GI tract and in some cases the skin. Unlike other systemic mycoses, candidiasis results from endogenous organisms. Most infections are brought on by C. albicans; however, C. glabrata (formerly Torulopsis glabrata) and other non-albicans species are increasingly associated with fungemia, UTIs, and, sometimes, other focal disease. C. glabrata is often less vulnerable to fluconazole than other types; C. krusei is inherently resistant to fluconazole; frequency of resistance to voriconazole and amphotericin varies. C. krusei is most frequently susceptible to echinocandins.
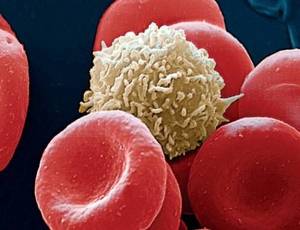
Candida sp represent about 80% of major systemic fungal infections and are the most typical reason for fungal infections in immunocompromised patients. Candidal infections are one of the most typical hospital-acquired infections. Because resistance and transmission of C. auris in healthcare facilities have actually become a concern, special infection control safety measures have been instituted for patients who are colonized or infected with C. auris.
Candidiasis of the esophagus is a defining opportunistic infection in AIDS. Although mucocutaneous candidiasis is often present in HIV-infected patients, hematogenous dissemination is unusual unless other particular risk factors exist.
Disseminated Candidiasis
Neutropenic patients (eg, those getting cancer chemotherapy) are at high risk of developing deadly distributed candidiasis. Candidemia may happen in nonneutropenic patients during extended hospitalization. This blood stream infection is frequently related to one or more of the following:
- Central venous catheters
- Significant surgery
- Broad-spectrum antibacterial therapy
- IV hyperalimentation
- IV lines and the GI tract are the usual portals of entry.
Candidemia often lengthens hospitalization and increases death due to concurrent disorders. Candidemia might accompany other types of invasive candidiasis, such as endocarditis or meningitis, as well as focal participation of skin, subcutaneous tissues, bones, joints, liver, spleen, kidneys, eyes, and other tissues. Endocarditis is frequently connected to IV substance abuse, valve replacement, or intravascular trauma induced by indwelling IV catheters.
All kinds of disseminated candidiasis must be considered severe, progressive, and potentially deadly.
Invasive Candidiasis Symptoms and Signs
Esophageal candidiasis is usually manifested by dysphagia.
Candidemia generally causes fever, but no symptoms are specific. Some patients develop a syndrome looking like bacterial sepsis, with a fulminating course that may include shock, oliguria, renal shutdown, and shared intravascular coagulation.
Candidal endophthalmitis starts as white retinal lesions that are at first asymptomatic however can progress, opacifying the vitreous and causing potentially permanent scarring and blindness. In neutropenic patients, retinal hemorrhages sometimes likewise occur, but actual infection of the eye is unusual.
Papulonodular skin sores may likewise establish, particularly in neutropenic patients, in whom they suggest prevalent hematogenous dissemination to other organs. Symptoms of other focal or intrusive infection depend on the organ included.
Diagnosis
- Histopathology and fungal cultures
- Blood cultures
- Serum beta-glucan testing
Due to the fact that Candida spp are commensal, their culture from sputum, the mouth, the vaginal area, urine, stool, or skin does not necessarily signify an intrusive, progressive infection. A particular medical lesion must likewise exist, histopathologic evidence of tissue invasion (eg, yeasts, pseudohyphae, or hyphae in tissue specimens) must be recorded, and other etiologies must be left out. Positive cultures of specimens drawn from usually sterilized sites, such as blood, CSF, pericardium, pericardial fluid, or biopsied tissue, offer definitive evidence that systemic therapy is required.
Serum beta-glucan is typically positive in patients with invasive candidiasis; alternatively, a negative result suggests low likelihood of systemic infection.
Ophthalmologic examination to look for endophthalmitis is recommended for all patients with candidemia.
Requirement laboratory methods often misidentify C. auris as C. haemulonii, C. famata, C. sake, or another types. Matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) is a more reliable technique for right identification.
Treatment
- An echinocandin if patients are seriously or seriously ill or if infection with C. glabrata, C. auris, or C. krusei is suspected
- Fluconazole if patients are medically steady or if infection with C. albicans or C. parapsilosis is presumed
- Additionally, voriconazole or amphotericin B.
Invasive Candidiasis
In patients with invasive candidiasis, inclining conditions (eg, neutropenia, immunosuppression, use of broad-spectrum anti-bacterial antibiotics, hyperalimentation, presence of indwelling lines) need to be reversed or managed if possible.
In nonneutropenic patients, IV catheters should be eliminated.
When an echinocandin is indicated (if patients are moderately badly ill or critically ill [most neutropenic patients] or if C. glabrata, C. auris, or C. krusei is presumed), among the following drugs can be used:
- Caspofungin, loading dose 70 mg IV, then 50 mg IV once/day.
- Micafungin 100 mg IV once/day.
- Anidulafungin, packing dosage 200 mg IV, then 100 mg IV once/day.
- If fluconazole is suggested (if patients are clinically steady or if C. albicans or C. parapsilosis is believed), filling dose is 800 mg (12 mg/kg) po or IV once, followed by 400 mg (6 mg/kg) once/day.
- If there is intolerance, restricted accessibility, or resistance to other antifungal drugs, a lipid formulation of amphotericin B at a dosage of 3 to 5 mg/kg IV once/day can be used (1).
Treatment of invasive candidiasis is continued for 14 days after the last unfavorable blood culture.
Esophageal Candidiasis
- Esophageal candidiasis is treated with among the following:.
- Fluconazole 200 to 400 mg po or IV once/day.
- Itraconazole 200 mg po once/day.
- If these drugs are ineffective or if infection is severe, one of the following might be used:.
- Voriconazole 4 mg/kg po or IV quote.
- Posaconazole 400 mg po bid.
- An echinocandin.
Treatment of esophageal candidiasis is continued for 14 to 21 days.