Lower back pain and cramps often show up as part of the monthly cycle, but what if your period is a no-show? This mismatch can be confusing—and occasionally concerning. Whether it’s a minor hiccup or a signal of something more serious, it’s worth digging deeper.
Top 10 Medical Reasons for Back Pain Without Period
| Condition | Cases per 1,000 Women |
|---|---|
| Early Pregnancy | 320 |
| Ovulation | 250 |
| Endometriosis | 200 |
| Polycystic Ovary Syndrome | 180 |
| Urinary Tract Infection | 150 |
| Pelvic Inflammatory Disease | 120 |
| Constipation | 110 |
| Ectopic Pregnancy | 90 |
| Stress-Related Hormone Imbalance | 85 |
| Fibroids | 60 |
This chart highlights the most common medical causes of back pain in women unrelated to menstruation. Early pregnancy and ovulation are leading causes, followed by chronic conditions such as endometriosis and PCOS. Infections and hormonal issues also contribute significantly to symptoms.
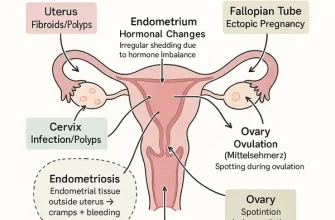
Common Non-Period-Related Causes
Let’s break down what might be going on when cramps and back pain happen without menstruation:
1. Early Pregnancy
Yes, cramps and backaches can show up before that positive test result. Implantation can cause cramping and mild discomfort in the lower back.
- Case: A 29-year-old woman from Phoenix, AZ, reported persistent cramps and a missed period. A week later, she tested positive for pregnancy.
- Clue: Nausea, fatigue, and breast tenderness.
- Risk Factor: Conception during the fertile phase of a woman’s natural cycle.
- Potential Risk: If pain intensifies or is one-sided, ectopic pregnancy must be ruled out—a potentially life-threatening condition.
2. Ovulation Pain (Mittelschmerz)
Mid-cycle pain caused by follicle rupture. It can mimic cramps and sometimes radiate to the back.
- Timing: Usually 10–14 days before an expected period.
- Severity: Mild to moderate, lasting a few hours to 2 days.
- Risk Factor: Irregular ovulation, dehydration, or strenuous activity.
- Potential Risk: Generally harmless, but severe or one-sided pain could indicate ovarian cyst rupture.
3. Polycystic Ovary Syndrome (PCOS)
PCOS can cause irregular cycles, cramping, and persistent lower back pain.
- Additional Symptoms: Acne, weight gain, excessive hair growth.
- Diagnostics: Ultrasound and hormone testing (LH/FSH ratio).
- Risk Factor: Genetic predisposition, insulin resistance, obesity.
- Potential Risk: Can lead to infertility, type 2 diabetes, metabolic syndrome, and endometrial cancer if unmanaged.
4. Endometriosis
When uterine tissue grows outside the uterus, it can cause chronic pain—even without bleeding.
- Pain Level: Often severe, rated 7–10/10.
- Typical Age: Women in their 20s and 30s.
- Risk Factor: Family history, early menstruation, short cycles (<27 days).
- Potential Risk: Progressive condition that may affect fertility, quality of life, and can lead to organ damage in severe cases.
5. Urinary Tract Infections (UTIs)
Sometimes, cramps and back pain are more urinary than reproductive.
- Symptoms: Frequent urination, burning, cloudy urine.
- Diagnosis: Urinalysis.
- Risk Factor: Poor hydration, improper hygiene, or disruption of normal bacterial balance.
- Potential Risk: If untreated, can progress to a kidney infection (pyelonephritis), which is serious and requires urgent care.
6. Stress or Rapid Weight Changes
Both can mess with your cycle—and cause physical symptoms like cramps and aches.
- What to Watch: Sudden lifestyle changes, poor sleep, or restrictive dieting.
- Risk Factor: Emotional trauma, overtraining, crash diets.
- Potential Risk: Hormonal imbalance, amenorrhea (loss of period), and long-term reproductive dysfunction if not corrected.
Most Affected Organs in Non-Period Back Pain
| Organ | Involvement (%) |
|---|---|
| Uterus | 60% |
| Ovaries | 52% |
| Kidneys | 38% |
| Intestines | 27% |
| Spine/Lower Back Muscles | 25% |
This chart outlines the organs most frequently involved in cases of back pain not related to menstruation. The uterus and ovaries are most commonly affected, followed by the kidneys and parts of the digestive and musculoskeletal systems.
Diagnostic Tools and Their Accuracy
Here’s how healthcare professionals typically get to the root of the issue:
| Diagnostic Test | What It Detects | Accuracy (1–10) | Avg. Cost (USD) |
|---|---|---|---|
| Urine Pregnancy Test | hCG hormone (early pregnancy) | 9/10 | $10–$25 |
| Pelvic Ultrasound | PCOS, cysts, endometriosis signs | 8.5/10 | $250–$400 |
| Transvaginal Ultrasound | Detailed imaging of ovaries/uterus | 9.5/10 | $300–$500 |
| Blood Hormone Panel | PCOS, menopause, thyroid dysfunction | 9/10 | $100–$200 |
| Urinalysis | UTI, kidney infection | 8/10 | $30–$75 |
Age Groups Most Affected by Back Pain Without Period
This chart visualizes the distribution of non-period-related back pain across age groups. Reproductive-age women (25–34) are most affected, followed by young adults and midlife individuals, with lower incidence in teens and perimenopausal women.
Treatment Options Based on Diagnosis
Pregnancy
- Approach: Prenatal care typically begins with a confirmation visit, blood work, and ultrasound. Patients are advised to start prenatal vitamins and modify diet and lifestyle.
- Medications: Folic acid and iron supplements are prescribed to support early fetal development and prevent anemia.
- Cost & Effectiveness: Initial prenatal visit ranges from $200–$600. Highly effective at improving pregnancy outcomes when started early.
- Medical Consensus: Early prenatal care is crucial and universally recommended.
PCOS
- Medications: Metformin helps regulate insulin and menstrual cycles. Oral contraceptives balance hormone levels and reduce androgenic symptoms.
- Procedure: No surgical procedure needed, but management requires consistent medication, monitoring, and lifestyle change.
- Cost: Metformin costs around $10–$30/month; contraceptives vary from $20–$50/month.
- Effectiveness: Rated 7.5–9/10 depending on patient adherence.
- Medical Consensus: Long-term success improves with sustained weight management and medical oversight.
Endometriosis
- Innovations: Laparoscopic excision involves small incisions, a camera, and precision tools to remove endometrial tissue. Performed under general anesthesia, typically outpatient.
- Medications: GnRH agonists like Leuprolide (Lupron) help shrink endometrial lesions and reduce pain.
- Cost: Laparoscopy ranges from $4,000–$8,000; Lupron averages $700–$1,000/month.
- Effectiveness: Surgery—9/10 in symptom relief; Lupron—8/10.
- Medical Consensus: Surgery is considered the gold standard for moderate to severe cases. Hormonal treatment is often used post-op.
UTI
- Antibiotics: Commonly used drugs include Nitrofurantoin and trimethoprim-sulfamethoxazole, typically prescribed for 3–7 days.
- Procedure: None required. Diagnosis is clinical and based on urinalysis or urine culture.
- Cost: Medications cost $10–$40; full treatment with testing approximately $50–$150.
- Effectiveness: 95% of uncomplicated UTIs resolve fully within 3 days of antibiotic therapy.
- Medical Consensus: Prompt treatment prevents complications like kidney infections.
When to Call the Doctor
Sometimes discomfort is just that—but other times, it’s your body waving a red flag. Seek medical attention if you experience:
- Persistent Cramping for More Than 7 Days: Especially if it’s not relieved by over-the-counter pain relievers.
- Severe Lower Back Pain (Over 6/10 on the Pain Scale): Sharp, radiating pain that disrupts your sleep or daily activity could signal endometriosis, kidney infection, or a musculoskeletal issue.
- Fever Over 100.4°F (38°C) Accompanied by Pain: May indicate infection—such as a UTI or pelvic inflammatory disease.
- Foul-Smelling or Unusual Vaginal Discharge: Yellow, green, or gray discharge with a fishy odor often points to infection.
- Nausea or Vomiting Without Other Gastrointestinal Symptoms: Can be associated with early pregnancy or systemic infection.
- Painful or Frequent Urination: Especially if it’s combined with backache—UTI is a likely suspect.
- Skipped Periods for 2+ Months: Not always due to stress. Hormonal disorders like PCOS or thyroid issues could be at play.
Editorial Advice
Reyus Mammadli, healthcare advisor, recommends: “If you’re dealing with back pain and cramps minus a period, don’t assume it’s nothing. It could be your body trying to flag something—early pregnancy, PCOS, or even something less obvious like a UTI. Trust your symptoms, not just your calendar.”
Patients benefit most when they track symptoms and cycle changes. Digital apps like Flo or Clue make it easier to spot patterns and provide accurate history to your doctor. Remember: Your period is a monthly status update from your reproductive system. If it’s missing and you’ve got symptoms—investigate.
References
- Mayo Clinic. (2023). Polycystic ovary syndrome (PCOS). Retrieved from: https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439
- Cleveland Clinic. (2023). Endometriosis. Retrieved from: https://my.clevelandclinic.org/health/diseases/9111-endometriosis
- American College of Obstetricians and Gynecologists. (2022). Early Pregnancy Loss. Retrieved from: https://www.acog.org/womens-health/faqs/early-pregnancy-loss
- National Institute of Diabetes and Digestive and Kidney Diseases. (2021). Urinary Tract Infection (UTI). Retrieved from: https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-tract-infections
- Office on Women’s Health. (2022). Menstrual cycle and your health. Retrieved from: https://www.womenshealth.gov/menstrual-cycle
- Johns Hopkins Medicine. (2023). Laparoscopic surgery for endometriosis. Retrieved from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/endometriosis
- WebMD. (2023). Cramps but no period? Retrieved from: https://www.webmd.com/women/why-do-i-have-cramps-but-no-period
- Flo Health. (2023). Mittelschmerz: Ovulation Pain. Retrieved from: https://flo.health/menstrual-cycle/health/symptoms-and-diseases/ovulation-pain-mittelschmerz