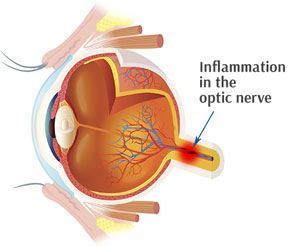
Optic neuritis is a swelling of the optic nerve, the bundle of nerve fibers that transfers visual details from your eye to your brain. Pain and temporary vision loss prevail symptoms of optic neuritis.
Optic neuritis is extremely related to multiple sclerosis, a disease that causes inflammation and damage to nerves in your brain and spinal cord. In some individuals, symptoms and signs of optic neuritis may be the first sign of multiple sclerosis.
Most people who have a single episode of optic neuritis ultimately recover their vision. Treatment with steroid medications might speed up vision recovery after optic neuritis.
Optic Neuritis Symptoms
Optic neuritis normally influences one eye. Symptoms may include:
- Pain. Most individuals who establish optic neuritis experience eye pain that’s worsened by eye movement. In some cases the pain feels like a dull ache behind the eye.
- Vision loss. Most individuals experience a minimum of some temporary reduction in vision, however the degree of vision loss varies. Noticeable vision loss normally develops over hours or days. Workout or a hot bath or shower may overemphasize the vision loss. Vision loss is irreversible in some cases.
- Loss of color vision. Optic neuritis commonly affects color understanding. You might observe that colors appear less brilliant than normal.
Flashing lights. Some individuals with optic neuritis credit report seeing flashing or flickering lights.
When to see a doctor
Eye conditions can be serious. Some can result in long-term vision loss, and some are connected with other severe medical issues. Contact your doctor if:
- You establish new symptoms, such as eye pain or a modification in your vision.
- Your symptoms aggravate or do not improve with treatment.
- You have unusual symptoms, consisting of tingling or weak point in one or more limbs, which may be a sign of a neurological disorder.
Causes
The exact reason for optic neuritis is unknown. However, optic neuritis is thought to establish when the body immune system incorrectly targets the compound covering your optic nerve (myelin), leading to inflammation and damage to the myelin.
Normally, the myelin assists electrical impulses travel rapidly from the eye to the brain, where they’re transformed into visual information. Optic neuritis disrupts this process, influencing vision.
The following autoimmune conditions commonly are related to optic neuritis:
Multiple sclerosis. Multiple sclerosis is an illness where your autoimmune system assaults the myelin sheath covering nerve fibers in your brain and spinal cord. In people with optic neuritis, the danger of establishing multiple sclerosis following one episode of optic neuritis has to do with 50 percent over a lifetime.
Your threat of developing multiple sclerosis after optical neuritis increases further if an MRI scan programs lesions on your brain.
Neuromyelitis optica. In this condition, swelling happens in the optic nerve and spinal cord. Neuromyelitis optica has resemblances to numerous sclerosis, however neuromyelitis optica does not cause damage to the nerves in the brain as often as multiple sclerosis does. Optic neuritis emerging from neuromyelitis optica tends to be more severe than optic neuritis associated with multiple sclerosis.
Other autoimmune conditions, such as sarcoidosis and systemic lupus erythematosus, have likewise been associated with optic neuritis.
Other aspects that have been linked to the development of optic neuritis consist of:
- Infections. Bacterial infections, including Lyme disease, cat-scratch fever and syphilis, or viruses such as measles, mumps and herpes can trigger optic neuritis.
- Drugs. Some drugs have been related to the development of optic neuritis. Among these drugs is ethambutol (Myambutol), which is used to treat tuberculosis.
Risk factors
Risk elements for optic neuritis arising from autoimmune disorders include:
- Age. Optic neuritis frequently affects young adults ages 20 to 40 years.
- Sex. Women are much more most likely to develop optic neuritis than men are by a ratio of 3-to-1.
- Race. In the United States, optic neuritis occurs more often in whites than it carries out in blacks.
- Genetic anomalies. Certain genetic anomalies may enhance your threat of developing optic neuritis or several sclerosis.
Complications arising from optic neuritis might consist of:
- Optic nerve damage. Many people have some irreversible optic nerve damage following an episode of optic neuritis, but the damage may not trigger symptoms.
- Decreased visual skill. Most individuals restore normal or near regular vision within a number of months. Nevertheless, a partial loss of color discrimination might continue. For some people, vision loss might persist after the optic neuritis has enhanced.
- Side effects of treatment. Steroid medications utilized to deal with optic neuritis suppress your immune system, which causes your body to end up being more prone to infections. Long-term use of steroids may likewise trigger other conditions such as thinning of your bones (osteoporosis).
If you have signs and symptoms of optic neuritis, you’ll likely see your family physician or a family doctor. However, you might be referred immediately to a doctor who specializes in diagnosing and dealing with eye diseases (ophthalmologist).
Here’s some information to help you get ready for your consultation and understand what to get out of your doctor.
What you can do before visit a doctor
- Write down any symptoms you’re experiencing, and for how long. Explain your symptoms as specifically as possible, consisting of score the seriousness of your vision loss and whether you see colors in a different way.
- Write down vital individual info, consisting of any current stress factors or major life modifications.
- Make a list of your key medical details. Your doctor will would like to know about any recent infectious illnesses you’ve had, as well as any other conditions with which you’ve been diagnosed. Also write down the names of all prescription and over-the-counter medications and supplements you’re taking.
- Take a family member or friend along. Someone who accompanies you can assist you bear in mind info your doctor provides you.
- Write down concerns to ask your doctor.
Preparing a list of concerns will assist you take advantage of your time with your doctor. For optic neuritis, concerns to ask your doctor include:
What is most likely causing my symptoms?
Are there other possible causes?
What tests do I need?
What treatments do you advise?
What are the possible side effects of the medications you’re suggesting?
How totally do you expect I will recover, and how long will that take?
How will you monitor my progress?
Does this condition put me at threat of other medical conditions?
How will you assess my threat of related conditions?
If tests show that I’m at enhanced danger of other medical conditions, exist treatments that can help in reducing my risk?
Are hereditary elements connected with my condition? Are my relatives at risk?
Do you suggest genetic testing for my immediate household?
I have other health conditions. How can I best handle these conditions together?
Do you have pamphlets or other printed product I can take with me? What sites do you recommend?
What to anticipate from your doctor
Your doctor is most likely to ask you a number of concerns, such as:
When did you start experiencing symptoms?
How would you explain your symptoms?
How considerably has your vision decreased?
Do colors look less vibrant?
Have your symptoms altered with time?
Does anything seem to make your symptoms much better, or worse, such as exhausting exercise or a hot shower?
Have you observed issues with movement and coordination?
Have you noticed pins and needles or weak point in your arms or legs?
Have you recently had an infection?
Have you been identified for other medical conditions?
Have any close relatives been detected with optic neuritis?
Have any close loved ones been diagnosed with several sclerosis?
Tests and medical diagnosis
You’re likely to see an ophthalmologist for a diagnosis, which is typically based upon your medical history and a test. The eye doctor likely will perform the following eye tests:
- A regular eye test. Your optometrist will check your vision and your ability to view colors.
- Ophthalmoscopy. During this evaluation, your doctor shines a brilliant light into your eye and examines the structures at the back of your eye. This eye test evaluates the optic disk, where the optic nerve gets in the retina in your eye. The optic disk ends up being inflamed in about one-third of individuals with optic neuritis.
- Pupillary light reaction test. Your doctor might move a flashlight in front of your eyes to see how your pupils react when they’re exposed to bright light. Pupils in eyes influenced by optic neuritis don’t constrict as much as those in healthy eyes do when stimulated by light.
Other tests to diagnose optic neuritis may consist of:
- Visual stimulated reaction. Throughout this test, you sit prior to a screen on which an alternating checkerboard pattern is displayed. Attached to your head are wires with little patches to tape your brain’s reactions to the visual stimuli. This kind of test spots the slowing of electrical conduction resulting from damage to the optic nerve.
- Magnetic resonance imaging (MRI) scan. An MRI scan utilizes an electromagnetic field and pulses of radio wave energy making pictures of your body. Throughout an MRI to check for optic neuritis, you might be injected with a contrast solution to make the optic nerve and other parts of your brain more visible on the images.
An MRI is essential to determine whether there are broken areas (sores) in your brain, which indicate a high risk of establishing numerous sclerosis. An MRI can likewise eliminate other causes of visual loss, such as a tumor.
Blood tests. A blood test is available to look for antibodies for neuromyelitis optica. Individuals with severe optic neuritis might undergo this test to identify whether they’re likely to develop neuromyelitis optica.
Optic Neuritis Treatments and Drugs
Optic neuritis normally improves by itself. Sometimes, steroid medications are made use of to minimize swelling in the optic nerve. Possible side effects from steroid treatment include weight gain, state of mind modifications, indigestion and sleeping disorders.
Steroid treatment is normally provided by vein (intravenously). Intravenous steroid treatment may speed vision recovery, however it does not appear to influence the degree to which you’ll recuperate vision you’ve lost. Steroid treatment is also made use of to lower the danger of developing numerous sclerosis or slow its development.
When steroid treatment fails and severe vision loss continues, a treatment called plasma exchange therapy may assist some people recover their vision. However, researches have not validated that plasma exchange treatment is effective for optic neuritis.
Preventing multiple sclerosis
If you have optic neuritis, and you have two or more brain sores evident on MRI scans, you might gain from drugs that assist prevent multiple sclerosis. These injectable drugs, including interferon beta-1a (Avonex, Rebif) and interferon beta-1b (Betaseron, Extavia), are utilized to avoid or delay the development of multiple sclerosis in individuals at high danger of the illness.
Diagnosis
Most individuals restore near to normal vision within 12 months after an optic neuritis episode.
People with numerous sclerosis or neuromyelitis optica might have a greater danger of recurrent attacks of optic neuritis. Optic neuritis can recur in people without underlying conditions, but those individuals usually have a better long-lasting diagnosis for their vision than do people with numerous sclerosis or neuromyelitis optica.