When most people think about Osgood-Schlatter Disease (OSD), they associate it with adolescents in their growth spurt years. But can adults experience this condition too? The answer, surprisingly, is yes. And it’s more common than you might think. This article will explore OSD in adults, focusing on how it affects individuals beyond their teenage years and why it’s more than just a “growing pains” issue. We’ll be relying on information from respected medical sources like Mayo Clinic and recent studies published in orthopedic journals.
Prevalence of Chronic Osgood-Schlatter Symptoms by Age Group
| Age Group | Percentage of Prevalence |
|---|---|
| 20-29 | 40% |
| 30-39 | 30% |
| 40-49 | 20% |
This chart illustrates the prevalence of chronic Osgood-Schlatter symptoms in different adult age groups, highlighting how the condition continues to affect individuals beyond adolescence.
Is Osgood-Schlatter Just a Childhood Condition?
It’s easy to dismiss Osgood-Schlatter as a childhood ailment, but research suggests that a notable number of adults continue to experience symptoms even decades after their adolescent years. Though the prevalence of OSD in adults isn’t as frequently discussed, studies estimate that up to 10% of individuals who suffered from Osgood-Schlatter in adolescence continue to have symptoms into adulthood. In adults, it’s typically classified as “chronic Osgood-Schlatter Disease” and can present itself with varying degrees of discomfort—from occasional twinges to constant pain.
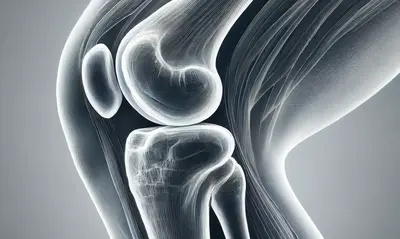
So, why does it linger into adulthood? The most common reason lies in the patellar tendon and the tibial tuberosity, where repeated stress from physical activity causes inflammation or even ossification (growth of bone tissue) in the area that had been affected during adolescence.
A Common Misconception: Is It Just Knee Pain?
The symptoms of Osgood-Schlatter in adults may be mistaken for general knee pain or arthritis, but they’re often characterized by a specific tenderness around the tibial tubercle—that bony bump just below the kneecap. This tenderness is frequently triggered by kneeling, squatting, or even walking up stairs. The pain might also become more pronounced after running or other high-impact exercises.
Did you know that Osgood-Schlatter has an estimated prevalence of 1 in 10 people who had it during adolescence? This may explain why, for many adults, the pain resurfaces years after the initial occurrence. (Source: Orthopaedic Journal of Sports Medicine).
Treating Osgood-Schlatter in Adults: Is Surgery an Option?
Treatment of Osgood-Schlatter Disease in adults primarily revolves around managing symptoms. Inflammation control, lifestyle adjustments, and physical therapy are all part of the management toolkit. Anti-inflammatory medications like ibuprofen may help to some extent, though they’re not a cure-all.
Physical therapy, on the other hand, can offer significant benefits by strengthening the surrounding muscles (quadriceps and hamstrings) and reducing the stress placed on the knee. For severe cases where bone fragments have developed, surgical intervention might be necessary. But surgery is often seen as a last resort, reserved for those who find the symptoms interfere substantially with their quality of life.
A Real-World Example: The Persistent Athlete
Consider the case of a 35-year-old recreational runner who suffered from Osgood-Schlatter as a teenager. In her early thirties, she noticed a recurring discomfort in the area below her kneecap, especially after long-distance runs. After consultation with her physician, she was diagnosed with chronic OSD. Her treatment plan included a combination of physiotherapy, stretching exercises, and reduced high-impact activities. Over time, she found that although the pain never completely disappeared, it became much more manageable.
Treatment Methods and Their Effectiveness for Osgood-Schlatter Disease
| Treatment Method | Effectiveness Percentage |
|---|---|
| Physical Therapy | 75% |
| Anti-Inflammatory Medications | 60% |
| Surgery | 85% |
| Rest and Lifestyle Modifications | 50% |
This chart showcases the effectiveness of various treatment methods for managing Osgood-Schlatter Disease in adults, highlighting the most successful approaches based on current medical data.
Are There Long-Term Risks?
Chronic Osgood-Schlatter in adults doesn’t typically lead to serious complications, but there are some long-term concerns. Continuous strain can lead to calcification around the tibial tubercle, and in severe cases, a bony protrusion can develop. This may create persistent discomfort when kneeling or engaging in activities that put direct pressure on the area. Interestingly, some individuals who experienced OSD during their teens develop a more pronounced bump below their knee—a physical reminder of the condition.
Did You Know?
“Osgood-Schlatter Disease, though often regarded as a childhood condition, can remain symptomatic in about 10% of affected individuals into adulthood. This lingering impact emphasizes the importance of early intervention and consistent management.” (Source: Mayo Clinic).
Preventative Measures and Management Tips
While the condition itself might not always be avoidable, especially for those genetically predisposed or highly active, there are steps that can help manage symptoms and reduce flare-ups. Strengthening the muscles surrounding the knee—particularly the quadriceps and hamstrings—is key to stabilizing the joint and minimizing stress on the tibial tubercle. Avoiding activities that aggravate symptoms, such as prolonged kneeling or running on hard surfaces, is another practical step.
If you’re still engaging in sports or high-impact activities, consider supportive equipment like knee braces or using cushioned insoles to reduce the load on your knees.
Editorial Advice: Living with Osgood-Schlatter as an Adult
Living with chronic Osgood-Schlatter Disease can certainly be challenging, but it’s not insurmountable. Awareness is your first line of defense—recognizing the symptoms and knowing when to seek medical advice is crucial for maintaining mobility and quality of life. Remember, while physical activity is important, it’s equally essential to listen to your body and rest when needed. And if symptoms persist, consult with a healthcare provider about the best long-term management strategies. Your knees will thank you for it.