Personalized medicine, often called precision medicine, has emerged as a revolutionary approach to healthcare, especially for chronic disease management. But what exactly makes it so effective? Let’s explore how personalized medicine is transforming the treatment of chronic illnesses, backed by facts, statistics, and real-world examples.
What is Personalized Medicine and Why Does it Matter?
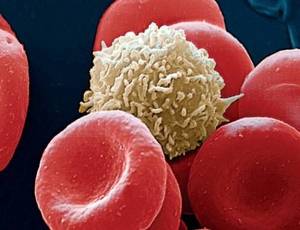
Have you ever wondered why two people with the same condition often respond differently to the same treatment? The answer lies in our unique genetics, lifestyles, and even microbiomes. Personalized medicine tailors treatment to the individual patient, utilizing genetic information, personal health history, and lifestyle to devise the most effective treatment plan.
The traditional “one-size-fits-all” approach to treating chronic conditions like diabetes, hypertension, and cancer is often ineffective and can lead to trial-and-error medication adjustments, potentially causing side effects. Personalized medicine aims to reduce these inefficiencies by offering a tailored solution. According to the National Institutes of Health (NIH), personalized medicine reduces hospitalization rates by up to 30% for some chronic illnesses.
How Personalized Medicine Changes the Game for Chronic Diseases
Chronic diseases account for about 90% of healthcare costs in the United States, with conditions like heart disease, cancer, and diabetes being the major culprits. What role does personalized medicine play here?
For diabetes management, for instance, tailored interventions can make a significant difference. Did you know that patients with type 2 diabetes who receive treatment tailored to their genetic makeup see a 50% improvement in glycemic control compared to those treated conventionally? This means fewer complications, a better quality of life, and, ultimately, reduced healthcare costs.
A study from the American Heart Association showed that patients with hypertension who had treatments personalized to their specific genetic markers experienced a 60% better response compared to those on standard treatment. This not only improves patient outcomes but also drastically reduces the time needed to find an effective treatment.
Did You Know?
Patients with chronic pain who receive personalized treatments based on genetic markers are 40% more likely to experience effective pain relief without escalating medication use. (Source: Mayo Clinic)
Leveraging Technology for Precision
Advancements in genomics, big data, and AI have made personalized medicine more accessible and actionable. Tools like genetic testing kits can help identify specific gene variants that may influence drug metabolism. For example, knowing whether a patient has a specific variant of the CYP2C9 gene can influence the dosage of blood thinners they need, avoiding dangerous overdoses or underdoses.
Moreover, wearable technology also plays a crucial role in personalized care. Devices that monitor heart rate, blood sugar, or physical activity levels allow healthcare providers to adjust treatment in real-time. These tools not only help physicians make informed decisions but also empower patients to take control of their health.
The Cost Factor: Is Personalized Medicine Affordable?
One of the common questions about personalized medicine is affordability. While it’s true that genetic testing and tailored treatment can be costly upfront, the overall savings in healthcare expenditure are substantial. For example, cancer patients receiving personalized treatments often avoid unnecessary chemotherapy, which can cost upwards of $10,000 per month. Reducing ineffective treatments ultimately saves patients and healthcare systems millions of dollars annually.
A report by McKinsey estimates that precision medicine could save the healthcare system $200 billion over the next 25 years by focusing on prevention and targeted intervention rather than reactive treatments. Additionally, pharmacogenetic testing—which helps determine the best drugs for a patient based on their genetic profile—can lead to a 30% reduction in adverse drug reactions, saving both lives and money.
Did You Know?
Adverse drug reactions account for over 100,000 deaths annually in the U.S., but personalized medicine could cut this number by a third. (Source: FDA)
Real-World Application: Oncology Leads the Way
Cancer treatment is where personalized medicine has made some of the biggest strides. In oncology, targeted therapies based on genetic information have significantly improved survival rates. For instance, patients with specific mutations in the EGFR gene are now treated with drugs that specifically target those mutations, resulting in a higher treatment success rate and fewer side effects.
One notable case is that of non-small cell lung cancer (NSCLC), where targeted treatments have increased five-year survival rates from 5% to nearly 25% over the past decade. By focusing on what makes each patient unique, oncologists can deliver treatments that are far more effective than traditional chemotherapy.
Personalized Medicine: A Patient-Centric Approach
Personalized medicine also emphasizes patient engagement. Patients are encouraged to participate in their treatment planning, which has been shown to improve compliance and outcomes. When patients understand why a certain medication works better for them—say, due to a genetic predisposition—they are more likely to follow through with the treatment.
For chronic diseases like rheumatoid arthritis, where medication adherence is crucial, personalized treatment plans have been linked to a 20% improvement in adherence rates. This means fewer flare-ups, lower hospital visits, and better disease management overall.
Impact of Personalized Medicine on Chronic Disease Management
Challenges and the Road Ahead
Despite its benefits, personalized medicine faces challenges. Genetic testing and data interpretation require specialized expertise, and there are still gaps in genetic data for certain populations. There’s also the ethical concern around data privacy—how do we ensure genetic information is used responsibly and securely?
However, the future looks promising. As technology advances and costs decrease, personalized medicine is expected to become the norm rather than the exception. Governments and healthcare institutions are increasingly investing in precision health initiatives, paving the way for a broader adoption of these life-changing practices.
Our Editorial Advice: If you or someone you know is managing a chronic condition, consider discussing personalized treatment options with your healthcare provider. With ongoing advancements in genetics and technology, these options are becoming more accessible and could offer a more effective path to managing chronic disease. Always stay informed, ask questions, and take an active role in your healthcare journey—your health is as unique as you are.