If you’re about to have your first root canal treatment, you may be feeling pretty apprehensive about the whole thing, particularly offered all the stories drifting around. Well, do not worry — all will be revealed in this detailed walk-through of root canal treatment. Knowing what will occur ahead of time is majority the battle; you will soon find out that it actually is much ado about nothing.
So let’s begin by eliminating a typical misconception: Root canal treatment does not cause pain– it alleviates it!
Introduction in Root Canal Procedure
A space inside the tooth called the pulp chamber homes the root canal system and pulp– the living tissue that keeps the tooth important (alive). The pulp consists of capillary, nerves and connective tissues, and, during childhood, develops the surrounding hard tissues of the tooth.
Endodontic treatment (” endo”– inside; “dont”– tooth), frequently referred to as root canal treatment, is needed when the pulp ends up being inflamed or infected. The causes could be deep dental caries, repeated dental procedures on one tooth (changing a large filling, for instance), or terrible damage such as a crack, chip or even a root fracture. Gum disease can also trigger root canal problems requiring root canal treatment.
Any of these issues can lead to severe inflammation of the pulp, which causes swelling and pressure inside the tooth (that has nowhere to go), causing tooth pain and, ultimately, irreversible damage to the pulp. Once the pulp dies, the pain might go away at first, often to return as an intense (painful) infection dispersing into the periapical tissues (” peri”– around; “apex”– end), particularly the bone. It might also become a chronic (long-standing) infection with symptoms varying from mild to severe.

Usually speaking, whatever the cause of root canal or pulpal disease, root canal or endodontic treatment will be necessary to conserve the tooth. All dentists get training in endodontic treatment and can carry out root canal procedures, however frequently a general dental practitioner will refer people who need endodontic treatment to an endodontist, a root canal expert.
Endodontists are dental experts who have completed an added two or more years of innovative residency training in the diagnosis and management of diseases and conditions of the dental pulp, and in the diagnosis of dental pain; their focus is for that reason on conserving teeth. In order to make an appropriate assessment and accurate diagnosis which tooth is affected and precisely what is triggering the pain, a thorough history and examination is required, together with a radiographic photo (x-ray) of the tooth or area.
Your dental practitioner or endodontist will inspect your medical history and present medications to guarantee your health and treatment safety. If you are really nervous, an oral sedative or anti-anxiety medication might be helpful– go over the alternatives with your dental expert or endodontist ahead of time.
How Long Does a Root Canal Take?
Over the last few decades, brand-new strategies and new types of equipment have been developed that have enhanced the efficiency with which endodontic therapy can be carried out. And this one reason why single-visit treatment is possible and has ended up being commonplace.
As a ballpark price quote, any single root canal appointment will typically last somewhere between 30 to 60 minutes and, in many cases, possibly as long as 90 minutes.
If you, as a patient, have a preference or a requirement for short visits (with the understanding that you will have to set up more of them) you should let your dentist know. This may include people who have TMJ (jaw-joint) problems or have problem sitting still for prolonged time periods.
On the other hand, some patients might have a strong preference or need for longer, yet fewer, consultations.
How many visits does root canal therapy take?
The number of appointments to it requires to finish your root canal treatment may be as few as one. With some cases, nevertheless, two or more scheduled consultations may be needed.
The two-visit approach
If two visits are required:
- The first is concentrated on the job of cleaning and forming the tooth’s root canal system.
- The second is used for filling and sealing the tooth.
- The two consultations are typically set up about a week apart.
Benefits of this method are that it makes managing any flare ups that develop easier and more predictable, and it also provides the dentist a chance to keep an eye on the progress of the tooth’s healing procedure.
Single-visit treatment
In the past, dental professionals always broke root canal therapy into two (or more) visits.
In the 1990’s the single-appointment approach began to acquire wide-spread acceptance, in part due to the fact that improvements in technology made it possible to complete a patient’s operate in a single sitting without jeopardizing treatment quality.
Step-By-Step Guide To Root Canal Procedure
Initial treatment to eliminate the decay and the source of infection of the pulp is necessary, together with a determination of whether the lost tooth structure can be restored. If a fracture of the tooth has reached the pulp, or infection is related to gum disease, it might be harder, if not impossible, to conserve the tooth.
The general sequence of a root canal procedure is as follows:
Step 1
Local anesthesia is administered by means of injections to numb the tooth to be treated and the surrounding tissues. If the pulp in a tooth is acutely irritated, and for that reason very painful, it may take a while to get it numb, however your dentist will not start the treatment till it is.
Step 2
A dental dam– a thin sheet of rubber or vinyl– will be placed over the impacted and surrounding teeth. The tooth going through treatment protrudes through a hole typed the dam, isolating it from the rest of the mouth. This allows the root canal treatment to be carried out in a sterilized environment free from contamination by bacteria found in saliva or the rest of the mouth.
Step 3
A small access hole is drilled through the biting surface of an impacted back tooth or from behind a front tooth, enabling access to the pulp chamber and root canals for treatment.
Step 4
The diseased and dead pulp tissue is removed from the tooth with specially developed instruments used to clear out the root canals and pulp chamber. This is not painful; the area is numb and the tissue being gotten rid of is either dead or dying. Once the pulp, in addition to the nerves consisted of in it, is removed, the tooth itself can no more feel pain.
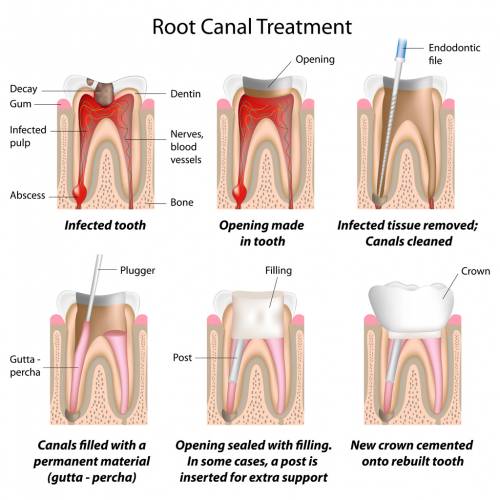
Step 5
The canals are decontaminated with antibacterial and antibacterial options.
Step 6
The canals are then formed with tiny flexible instruments to allow them to receive root canal fillings and sealants. The canals are washed and cleaned once again to get rid of root canal debris prior to sealing them.
Step 7
Root canal fillings are chosen that will exactly fit into the freshly ready canals. Typically a rubber-like material called gutta-percha is used to fill the canal area. It is a thermoplastic product (” thermo”– heat; “plastic”– to shape), which literally is heated and after that compressed into and against the walls of the root canals to seal them. Together with adhesive cement called a sealer, the gutta-percha fills the prepared canal area. Sealing the canals is critically essential to avoid them from becoming reinfected with bacteria.
Step 8
A temporary or long-term filling material will then be positioned to seal the access hole that was made to treat the canals, and the dental dam is gotten rid of. If the tooth lacks enough structure to hold a restoration (filling) in place, the dental expert or endodontist may place a post (either metal or an extremely strong plastic) in one of the canals inside the tooth to assist keep it.
Step 9
After the procedure, an antibiotic might be prescribed to treat or avoid infection. Be sure to follow the instructions of your dental professional or endodontist thoroughly. After-effects of treatment are minimal, generally lasting from a couple of days to about a week, according to iytmed.com. It is regular to have some minor discomfort after treatment consisting of minor soreness that can generally be handled with over the counter (aspirin, ibuprofen) medications or prescription (codeine-type) drugs, or a combination of the two.
Step 10
Your tooth will require a long-term remediation– a filling or a crown– to change lost tooth structure, and offer a total seal to the top of the tooth. Your endodontist will send you back to your basic dental practitioner to determine which type of restoration is best for you. This step is of specific importance given that many studies show that if the filled root canals are recontaminated with bacteria from the mouth, there could be a recurrence of infection around the tooth.
Bottom line
Nearly like the root system of a plant, the root canals of a tooth have a main branch and lots of smaller side branches, and the whole system has to be sealed during root canal treatment to be effective long term. Since root canals are very small areas, they need a lot of precision and care to treat well. Therefore, most endodontists today use modern technology consisting of digital (radiographic) imaging to detect root canal problems, and after treatment to verify that the canals are appropriately sealed; ultrasonic instrumentation to remove old canal fillings and posts and clean canals; and operating microscopes to accurately locate, visualize and seal root canal systems; it actually is quite state-of-the-art.








