The human body relies on a complex network of blood cells to maintain health, immunity, and overall functionality. These cells, each with unique characteristics and purposes, are fundamental to life. This article explores the three primary types of blood cells, their specific roles, and their importance in maintaining physiological balance.
Distribution of Blood Cells by Type
| Cell Type | Percentage |
|---|---|
| Red Blood Cells | 40-50% |
| White Blood Cells | <1% |
| Platelets | <1% |
This chart illustrates the proportional distribution of blood cell types in the human body, emphasizing the predominance of red blood cells, while white blood cells and platelets collectively account for less than 2% of blood volume.
1. Red Blood Cells (Erythrocytes)
Red blood cells (RBCs) are the most abundant type of blood cell, accounting for nearly 40-50% of blood volume in adults. These disc-shaped cells lack a nucleus, maximizing their capacity for carrying oxygen throughout the body.
- Primary Function: RBCs transport oxygen from the lungs to tissues and return carbon dioxide to the lungs for exhalation. This exchange of gases is critical for cellular respiration and energy production.
- Key Protein: Hemoglobin, an iron-rich protein, binds oxygen molecules in the lungs and releases them to tissues. Hemoglobin also facilitates the removal of carbon dioxide, a waste product of metabolism.
- Lifespan: Approximately 120 days before being replaced by new cells produced in the bone marrow, a process regulated by the hormone erythropoietin.
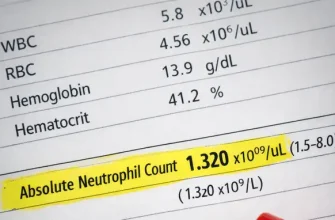
How RBC Levels Are Measured
RBC levels are assessed through a complete blood count (CBC) test, which measures the number of red blood cells per microliter of blood. Additionally, the test evaluates hemoglobin levels and hematocrit (the proportion of red blood cells in the blood). Normal ranges are approximately 4.7 to 6.1 million cells/µL for men, 4.2 to 5.4 million cells/µL for women, and 4.1 to 5.5 million cells/µL for children.
Importance in Medicine
Maintaining healthy RBC levels is vital for preventing conditions like anemia, characterized by low RBC or hemoglobin levels. This condition can lead to fatigue, shortness of breath, and poor oxygen delivery to tissues. Elevated RBC levels, known as polycythemia, can increase the risk of blood clots. Monitoring RBC counts helps diagnose and manage disorders, assess treatment efficacy, and ensure adequate oxygenation in critical care settings.
Real-Life Case
A 35-year-old woman from Texas experienced chronic fatigue and shortness of breath. Blood tests revealed her hemoglobin levels were significantly low, indicating anemia. Iron supplements and dietary adjustments restored her RBC count and energy levels.
2. White Blood Cells (Leukocytes)
White blood cells (WBCs) are the immune system’s defenders, accounting for less than 1% of blood volume. Despite their smaller quantity, their role is indispensable for protecting the body against infections and foreign invaders. Their functionality is monitored through a complete blood count (CBC) test, which provides the total number of WBCs and a breakdown of their types. The normal range for WBC count is 4,000 to 11,000 cells per microliter of blood, and any deviation could indicate underlying conditions such as infection, inflammation, or immune system disorders.
- Types of WBCs:
- Neutrophils: First responders to bacterial infections. They form pus and are a key indicator of acute infections.
- Lymphocytes: Key players in producing antibodies and regulating immune responses, especially against viruses.
- Monocytes: Aid in cleaning up dead cells and pathogens, and they differentiate into macrophages in tissues.
- Eosinophils: Combat parasitic infections and play a role in allergic responses, often elevated in conditions like asthma.
- Basophils: Release histamine during allergic reactions and help mediate inflammatory responses.
- Lifespan: Ranges from hours for neutrophils to several years for lymphocytes, depending on the type.
Importance in Medicine
WBC levels are a crucial diagnostic marker. Elevated counts, known as leukocytosis, can indicate infections, chronic inflammation, or even leukemia. Conversely, low counts, or leukopenia, may result from conditions like bone marrow disorders or autoimmune diseases. Understanding WBC counts helps in diagnosing and monitoring treatment efficacy for various illnesses. For instance, a decrease in neutrophils (neutropenia) can significantly heighten the risk of infections, especially in cancer patients undergoing chemotherapy.
Real-Life Case
A 10-year-old boy from Florida developed recurring fevers and swollen lymph nodes. Blood tests showed elevated WBC levels, leading to a diagnosis of acute lymphoblastic leukemia. Early intervention and chemotherapy achieved remission.
3. Platelets (Thrombocytes)
Platelets are small, disc-shaped cell fragments that play a crucial role in blood clotting and wound healing. When a blood vessel is injured, platelets are among the first responders, forming a plug to prevent excessive bleeding and starting the healing process.
- Primary Function: Platelets detect damage in blood vessel walls and adhere to the site of injury. They release chemical signals that attract more platelets and initiate the coagulation cascade, a series of steps involving clotting factors that stabilize the wound.
- Key Process: Their action begins with adhesion to the damaged area, followed by aggregation into a platelet plug. This is reinforced by fibrin, a protein that creates a durable clot.
- Lifespan: Approximately 7-10 days, after which they are removed by the spleen and liver.
Measuring platelet levels involves a complete blood count (CBC) test, a standard diagnostic tool in medicine. The normal range is typically 150,000 to 450,000 platelets per microliter of blood. Deviations from this range can indicate conditions such as thrombocytopenia (low platelet count) or thrombocytosis (high platelet count), which may lead to bleeding disorders or clotting complications.
Importance in Medicine
Platelets are vital in surgeries and trauma care, where controlling bleeding is critical. They are also central to the management of clotting disorders, such as hemophilia, and monitoring cardiovascular health. Advances in platelet research have led to innovative treatments, including platelet-rich plasma (PRP) therapy, which is used in wound healing and tissue regeneration.
Real-Life Case
A 50-year-old man in California underwent surgery and experienced prolonged bleeding. Tests revealed thrombocytopenia (low platelet count). A platelet transfusion stabilized his condition, allowing the healing process to proceed.
Table: Overview of Blood Cells
| Blood Cell Type | Primary Function | Average Lifespan |
|---|---|---|
| Red Blood Cells | Oxygen transport | ~120 days |
| White Blood Cells | Immune defense | Hours to years |
| Platelets | Blood clotting and wound healing | 7-10 days |
Normal Ranges of Blood Cell Counts
| Blood Cell Type | Normal Range |
|---|---|
| Red Blood Cells (RBC) | 4.2 – 6.1 million/µL |
| White Blood Cells (WBC) | 4,000 – 11,000/µL |
| Platelets | 150,000 – 450,000/µL |
This chart highlights the normal ranges of blood cell counts, which are critical for diagnosing and monitoring health conditions. Any deviations from these ranges could indicate underlying medical issues requiring further investigation.
Expert Insight
Reyus Mammadli, a healthcare advisor, emphasizes the importance of maintaining healthy blood cell levels. “A balanced diet rich in iron, vitamins B12, and folate supports red blood cell production, while adequate hydration and hygiene can protect white blood cell function. Platelets require a delicate balance, as too few can lead to bleeding, while too many may increase clotting risks.”
Common Disorders Related to Blood Cells
- Anemia: A condition characterized by low red blood cell count or hemoglobin levels, leading to fatigue and weakness. For example, a 22-year-old college student in New York experienced persistent tiredness and pale skin. Bloodwork showed iron deficiency anemia, which was resolved with dietary changes and supplements.
- Leukemia: A type of cancer affecting white blood cells, causing abnormal production and function. In one instance, a 45-year-old teacher from Illinois noticed unusual bruising and frequent infections. A diagnosis of chronic lymphocytic leukemia led to targeted therapy and symptom management.
- Thrombocytopenia: A disorder where platelet levels are too low, increasing the risk of excessive bleeding. A 60-year-old retired firefighter in Oregon developed severe nosebleeds and pinpoint red spots on his skin. A bone marrow biopsy confirmed immune thrombocytopenia, treated effectively with corticosteroids.
Stages of Blood Clotting
| Stage | Description |
|---|---|
| 1. Vascular Spasm | The blood vessel constricts to reduce blood flow to the injured area. |
| 2. Platelet Plug Formation | Platelets adhere to the damaged area and release chemical signals to recruit more platelets, forming a temporary plug. |
| 3. Coagulation Cascade | A series of enzymatic reactions activate clotting factors, leading to the conversion of fibrinogen into fibrin, which stabilizes the plug. |
| 4. Clot Retraction | The clot contracts to bring the wound edges closer, reducing the size of the injury. |
| 5. Clot Dissolution (Fibrinolysis) | Plasmin breaks down the clot once the vessel is healed, restoring normal blood flow. |
This chart outlines the stages of blood clotting, a critical process that prevents excessive bleeding and aids in tissue repair. Understanding these stages is essential for diagnosing and treating clotting disorders.
Editorial Advice
“Understanding the functions of blood cells can help individuals recognize potential health issues early,” says Reyus Mammadli. “Regular check-ups, a nutrient-rich diet, and timely medical care are vital for maintaining healthy blood cells. If you experience unusual symptoms like prolonged fatigue, frequent infections, or excessive bleeding, consult a healthcare provider promptly.”