What is Baastrup’s Disease? Baastrup’s Disease, also known as “kissing spine syndrome,” is a condition characterized by the abnormal contact between adjacent spinous processes in the spine. This contact causes inflammation and pain in the affected area. It commonly occurs in the lumbar or lower back region.
The main cause of Baastrup’s Disease is repetitive hyperextension and compression of the spine, often due to poor posture or degenerative changes in the spinal discs and joints.
Symptoms of this condition include localized back pain, stiffness, and tenderness at the site of contact. Diagnosis typically involves a physical examination, medical history review, and imaging tests such as X-rays or MRI scans. Treatment options range from conservative measures such as pain management and physical therapy to surgical interventions when necessary.
Definition and Сauses of Baastrup’s Disease
Baastrup’s Disease, also known as kissing spine syndrome or interspinous bursitis, is a condition characterized by the inflammation of the spinous processes in the lower back. The spinous processes are the bony projections that are visible along the back of the spine.
The exact cause of Baastrup’s Disease is not fully understood, but it is believed to be related to repetitive stress or injury to the lower back. This can occur due to factors such as poor posture, age-related degenerative changes in the spine, or excessive hyperextension of the lumbar region. Over time, the repetitive contact between adjacent spinous processes can lead to friction, inflammation, and pain.
How is Baastrup’s Disease Diagnosed?
To diagnose Baastrup’s Disease, a healthcare provider will typically begin with a physical examination and review of the patient’s medical history.
Physical examination and medical history for Baastrup’s Disease
During a physical examination for Baastrup’s Disease, the healthcare provider will typically conduct a thorough examination of the affected area, which is usually the lower back. They may look for any visible signs of inflammation or swelling in the bony prominences. The physician will also assess the patient’s range of motion and perform specific maneuvers to reproduce the characteristic pain associated with Baastrup’s Disease.
Additionally, a detailed medical history will be taken to understand the onset of symptoms, any previous injuries or surgeries, and any underlying health conditions that could contribute to the development of Baastrup’s Disease. This information helps in making an accurate diagnosis and formulating an appropriate treatment plan.
Diagnostic tests for Baastrup’s Disease
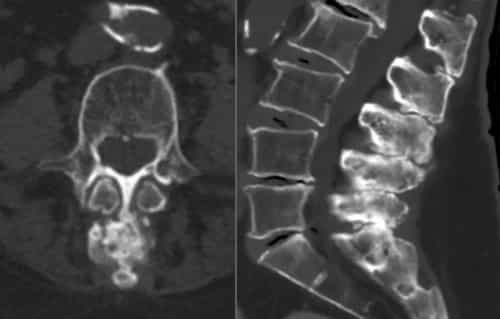
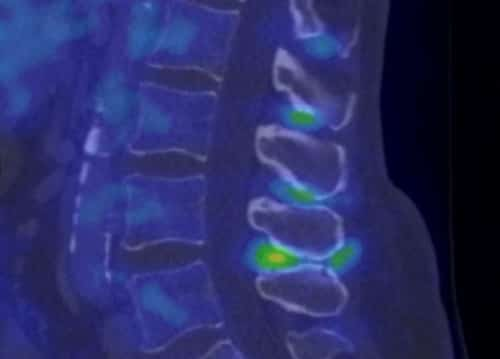
Diagnostic tests play a crucial role in confirming the presence of Baastrup’s Disease. One common diagnostic tool is imaging tests such as X-rays, MRI scans, or CT scans. These tests allow healthcare professionals to visualize the spine and identify any abnormalities or degenerative changes in the lumbar region.
X-rays can reveal degenerated discs, while MRI and CT scans provide more detailed images of the spine and allow for a closer examination of the bones, joints, and soft tissues. Additionally, diagnostic injections may be performed to determine if Baastrup’s Disease is the cause of the pain. These injections involve injecting a local anesthetic into the affected area to temporarily relieve pain and confirm the diagnosis.
What are the Common Symptoms of Baastrup’s Disease?
Common symptoms of Baastrup’s Disease typically include pain and discomfort in the lower back. This pain is often localized to the area around the spine and can be worsened by activities that involve bending or twisting the spine.
Individuals with Baastrup’s Disease may also experience tenderness or swelling in the affected area. In some cases, there may be a noticeable reduction in range of motion, making it difficult to perform certain movements. It is important to note that these symptoms can vary from person to person and may come and go over time.
If you are experiencing persistent back pain or any of these symptoms, it is advisable to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
Pain and discomfort associated with Baastrup’s Disease
Pain and discomfort are common symptoms associated with Baastrup’s Disease. Individuals with this condition often experience localized pain in the lower back region, specifically in the area where the spinous processes of adjacent vertebrae make contact. This pain can range from mild to severe and may be aggravated by certain movements or positions.
The discomfort is typically described as a deep, achy sensation that can become more intense with prolonged sitting or standing. Bending forward or backward may also exacerbate the pain. Additionally, individuals may experience stiffness and restricted range of motion in the spine.
It is important to note that the intensity of pain can vary among individuals, and some may experience periodic flare-ups where the pain becomes more pronounced.
Other symptoms and complications
Other symptoms of Baastrup’s Disease may include tenderness or swelling in the lower back area. Individuals may experience stiffness and limited range of motion, making it difficult to perform daily activities or engage in physical exercise.
In some cases, the condition can lead to muscle weakness or atrophy, as well as nerve compression, causing radiating pain or numbness in the buttocks or legs. Baastrup’s Disease can also increase the risk of developing other spinal conditions, such as spinal stenosis or herniated discs. These complications can further exacerbate pain and discomfort, affecting an individual’s overall quality of life.
Treatment Options for Baastrup’s Disease
Non-surgical treatment methods for Baastrup’s Disease aim to alleviate pain and discomfort. These may include physical therapy, which focuses on strengthening the muscles surrounding the affected area and improving posture. Heat or cold therapy, such as hot compresses or ice packs, can also help reduce inflammation and provide temporary relief.
Non-surgical treatment methods for Baastrup’s Disease
Non-surgical treatment methods for Baastrup’s Disease often focus on managing pain and addressing the underlying causes of the condition. Physical therapy can play a crucial role in alleviating symptoms by strengthening the muscles surrounding the spine and improving flexibility.
Techniques like manual therapy, stretching exercises, and postural correction can help relieve pain and discomfort. In addition, nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce inflammation and provide pain relief. Other treatment options may include the use of assistive devices like braces or orthotics to provide support to the spine.
Surgical options for Baastrup’s Disease
Surgical intervention may be considered for patients who do not respond to non-surgical treatments or for those with severe Baastrup’s Disease symptoms. The surgical options for Baastrup’s Disease aim to alleviate pain and improve spinal function.
One common surgical procedure is decompression surgery, which involves the removal of excessive bone growth and damaged tissue around the affected area. This relieves pressure on the spinous processes and neighboring structures, reducing pain and discomfort.
Another surgical option is spinal fusion, in which the affected vertebrae are fused together using bone grafts or metal implants. This procedure stabilizes the spine and restricts movement, allowing for healing and pain reduction.
Can Baastrup’s Disease be Prevented?
Preventive measures for Baastrup’s Disease include maintaining good posture and body mechanics, as well as ensuring proper spine alignment. It is important to avoid excessive strain and repetitive movements that can contribute to the development of the condition.

Preventive measures for Baastrup’s Disease
To prevent Baastrup’s Disease, there are a few measures that individuals can take. One important preventive measure is to maintain proper posture and body mechanics when performing activities that put strain on the spine. This includes lifting heavy objects with a straight back and avoiding excessive bending or twisting motions.
Regular exercise and strengthening the core muscles can also help support the spine and reduce the risk of developing Baastrup’s Disease. Maintaining a healthy weight is crucial, as excess weight can put additional stress on the spine.
Additionally, avoiding repetitive movements that strain the lower back and practicing good ergonomics at work can also contribute to preventing this condition.
Lifestyle changes to reduce the risk of Baastrup’s Disease
Maintaining a healthy lifestyle can play a crucial role in reducing the risk of developing Baastrup’s Disease. Here are some lifestyle changes that individuals can consider:
- Engage in regular physical activity: Regular exercise helps to strengthen the muscles supporting the spine, reducing strain on the spine and decreasing the likelihood of developing Baastrup’s Disease.
- Practice good posture: Maintaining proper posture while sitting, standing, and lifting can help prevent excessive stress on the spine and reduce the chances of Baastrup’s Disease.
- Take breaks during prolonged sitting or standing: Frequent breaks during prolonged periods of sitting or standing can help alleviate pressure on the spine and minimize the risk of Baastrup’s Disease.
- Maintain a healthy weight: Excess weight places additional stress on the spine, increasing the risk of developing Baastrup’s Disease. Maintaining a healthy weight through a balanced diet and regular exercise is essential.
- Avoid repetitive movements or activities that strain the spine: Repeating certain movements or activities that place strain on the spine can contribute to Baastrup’s Disease. It is important to be mindful of these activities and take preventive measures, such as using proper techniques or equipment.
By incorporating these lifestyle changes into their routine, individuals can reduce their risk of developing Baastrup’s Disease and promote overall spinal health.
Is Baastrup’s Disease a Progressive Condition?
Baastrup’s Disease is not considered a progressive condition in the traditional sense. It is a degenerative disorder that affects the spine, specifically the lumbar region. Unlike some progressive conditions where symptoms worsen over time, Baastrup’s Disease typically presents as a localized problem that can be managed through appropriate treatment and lifestyle modifications.
Understanding the progression of Baastrup’s Disease
Baastrup’s Disease is generally considered a progressive condition. Over time, the repetitive stress and friction between the spinous processes can lead to the development of bone spurs, also known as osteophytes. These bony growths can increase in size and cause more discomfort and pain for individuals with Baastrup’s Disease.
As the disease progresses, it can also lead to further complications such as nerve compression or spinal stenosis. This may result in radiating pain, numbness, or weakness in the affected area. In some cases, the progression of Baastrup’s Disease may necessitate more aggressive treatment options such as surgery to alleviate symptoms and prevent further deterioration.
Long-term effects and prognosis
Long-term effects of Baastrup’s Disease can vary depending on the severity and progression of the condition. Chronic back pain and limited range of motion are common long-term effects, which can significantly impact daily activities and quality of life. If left untreated or improperly managed, Baastrup’s Disease can lead to degenerative changes in the spine, such as spinal stenosis or disc herniation.
Prognosis for Baastrup’s Disease is generally good with appropriate treatment. Non-surgical methods like physical therapy, pain management techniques, and lifestyle modifications can help alleviate symptoms and improve function. Surgical interventions may be necessary in more severe cases, offering long-term relief.
Are There Any Alternative Treatments for Baastrup’s Disease?
Alternative treatments can be considered for the management of Baastrup’s Disease, although their effectiveness may vary from person to person. Some alternative therapies that have been explored include chiropractic adjustments, physical therapy, and massage therapy.
Alternative therapies for Baastrup’s Disease
Some individuals may seek alternative therapies to manage the symptoms of Baastrup’s Disease. These alternative treatments include chiropractic care, and herbal remedies. Chiropractic care focuses on realigning the spine and relieving pressure on the affected area. Herbal remedies, such as arnica or turmeric, may also be used to reduce inflammation and alleviate discomfort.
While some people may find these alternative therapies helpful in managing their symptoms, it is important to note that there is limited scientific evidence supporting their effectiveness for Baastrup’s Disease specifically. Therefore, it is advisable to consult with a healthcare professional before pursuing these alternative treatments and to always follow their recommendations for comprehensive management of the condition.
Effectiveness and considerations
When it comes to alternative treatments for Baastrup’s Disease, there is limited scientific evidence to support their effectiveness. Some individuals may find relief through methods like chiropractic adjustment, massage therapy, or herbal remedies. However, it is important to keep in mind that each person’s response to these treatments may vary.
Before considering alternative therapies, it is crucial to consult with a healthcare professional who specializes in spinal conditions. They can provide guidance on the potential risks and benefits of these treatments and whether they are suitable for your specific situation.
It is also important to note that alternative treatments should not replace conventional medical care. They should be used as complementary approaches alongside conventional treatment methods to maximize the likelihood of symptom improvement and overall well-being. Always discuss any alternative treatment options with your healthcare provider before pursuing them.
Can Baastrup’s Disease Recur After Treatment?
Recurrence rates and factors for Baastrup’s Disease vary among individuals. While treatment can provide relief from symptoms, it is possible for the disease to recur after treatment. The recurrence of Baastrup’s Disease can be influenced by various factors, including the effectiveness of the initial treatment, underlying spinal conditions, and lifestyle habits.
To minimize the risk of recurrence, it is important to follow the recommended treatment plan and engage in preventive measures. Regular exercise, maintaining a healthy weight, practicing good posture, and avoiding excessive stress on the spine are all helpful in preventing the return of Baastrup’s Disease.
Furthermore, individuals who have been treated for Baastrup’s Disease should undergo regular follow-up appointments with their healthcare provider to monitor their condition and address any potential signs of recurrence. A proactive approach to managing this condition can significantly reduce the likelihood of it recurring after treatment.
Recurrence rates and factors for Baastrup’s Disease
Recurrence rates and factors for Baastrup’s Disease vary among individuals. While there is limited research on the specific recurrence rates, it has been observed that the condition may recur after treatment.
Factors that may contribute to the recurrence of Baastrup’s Disease include inadequate treatment, not addressing underlying conditions, poor posture, and lack of proper rehabilitation or follow-up care. It is important to note that prevention strategies such as maintaining good spinal alignment and practicing proper body mechanics can help reduce the risk of recurrence.
Additionally, if symptoms reoccur after treatment, it is advisable to seek medical attention promptly to prevent further complications and manage the condition effectively.
Prevention strategies and follow-up care
To prevent Baastrup’s Disease, it’s essential to adopt certain prevention strategies and follow-up care. Maintaining a healthy weight is crucial as excess weight can put additional stress on the spine. Regular exercise that focuses on strengthening the core muscles can also help in preventing this condition.
It is important to maintain good posture while sitting and standing to avoid excessive strain on the spine. Engaging in activities that promote flexibility, such as stretching exercises, can also be beneficial.
Regular follow-up care is necessary for individuals who have been diagnosed with Baastrup’s Disease. This may include periodic visits to a healthcare professional or physical therapist to monitor the progress of the condition and receive appropriate treatment if needed.
Conclusion
Baastrup’s Disease is a condition that causes pain and discomfort in the lower back due to excessive friction between adjacent spinous processes. It can be diagnosed through physical examination, medical history, and imaging tests. Treatment options include non-surgical methods such as physical therapy, pain management techniques, and lifestyle changes. In more severe cases, surgery may be recommended.
While there is no surefire way to prevent Baastrup’s Disease, taking preventive measures like maintaining good posture, practicing regular exercise, and avoiding excessive strain on the spine can help reduce the risk.
It is important to note that Baastrup’s Disease can vary in its progression and long-term effects. Regular follow-up care and adherence to preventive strategies are crucial in order to prevent recurrence.
Key takeaways from Baastrup’s Disease
- Baastrup’s Disease, also known as kissing spine syndrome, is a condition where the spinous processes of adjacent vertebrae come into contact and cause pain and inflammation.
- The main cause of Baastrup’s Disease is repetitive or excessive flexion/extension movements of the spine, leading to degenerative changes in the spinous processes.
- Common symptoms include back pain, stiffness, and limited mobility. Diagnosis involves a physical examination, medical history review, and diagnostic tests such as X-rays or MRIs.
- Non-surgical treatment options include physical therapy, pain management techniques, and posture correction exercises.
- Surgical interventions may be necessary in severe cases that do not respond to conservative treatments. These procedures aim to remove excess bone or realign the affected vertebrae.
Baastrup’s Disease is a degenerative condition of the spine that can cause significant discomfort and limited functionality. Treatment options range from non-invasive methods to surgical interventions, depending on the severity of the symptoms and response to conservative measures. Early diagnosis and appropriate management can help alleviate pain and improve quality of life for individuals with this condition. For more detailed information about Baastrup’s Disease, refer to trusted medical resources and consult with a healthcare professional specialized in spinal conditions.