Low hematocrit isn’t a diagnosis by itself—it’s a dashboard light. When Hct dips below normal, the blood carries less oxygen, tissues run on “backup power,” and symptoms creep in: fatigue, shortness of breath, dizziness. The good news? With the right testing sequence and targeted therapy, most people can turn this number around—often faster than they think. Here’s the deal: understanding why Hct is low is the entire ballgame.
Hematocrit (Hct): The Basics of the Blood Test
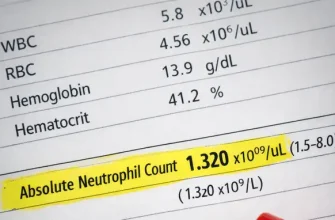
This section explains what hematocrit is and how it is measured. Hematocrit (Hct) is the percentage of your blood volume that’s made up of red blood cells (RBCs). It’s calculated from a Complete Blood Count (CBC). Labs either directly measure the packed cell volume or derive Hct from hemoglobin (Hb) and RBC indices. Because RBCs are the body’s oxygen couriers, a lower-than-expected Hct usually means your tissues get less oxygen—hence the classic “I’m wiped out” feeling.
Reference ranges vary slightly by lab and altitude, but commonly:
| Group | Typical Hct Range (%) |
|---|---|
| Adult men | 40.7–50.3 |
| Adult women | 36.1–44.3 |
| Newborns | 45–61 |
| Infants | 32–42 |
Normal ranges are context-dependent (e.g., smokers and those living at high altitudes may run higher). Full reference and patient-friendly explanations are available here ⧉.
Hydration status also matters. Overhydration can dilute Hct; dehydration can concentrate it. Recent blood loss may not immediately show as low Hct until plasma volume re-equilibrates. That’s why clinicians interpret Hct with hemoglobin, RBC count, and clinical context.
Normal Hematocrit Ranges by Age and Gender
This part outlines how different populations interpret their Hct. Ranges tighten or shift with age, sex, and pregnancy. For example, physiologic hemodilution in pregnancy lowers Hct, and pediatric values change across growth stages. Below is a practical, clinic-style snapshot (ballpark ranges; check your lab’s report for specifics):
| Population | Normal Hct (%) | Notes |
|---|---|---|
| Men (≥18 y) | ~41–50 | Endurance training and altitude can push higher |
| Women (≥18 y) | ~36–44 | Menstrual blood loss can nudge lower |
| 1–10 y | ~31–43 | Wide variation by age; use pediatric reference |
| Teens (F) | ~34–44 | Iron deficiency is common in menstruating teens |
| Pregnancy | ~32–37 | Physiologic hemodilution; trimester-specific cutoffs |
In U.S. population data from 2021–2023, anemia prevalence across ages ≥2 years was about 9.3%, reminding clinicians to keep an eye on CBC trends, not just one-off values ⧉.
What Does Low Hematocrit Mean?
Low Hct is not a disease but a signal. It usually reflects one (or a combo) of: not enough RBC production (e.g., iron/B12/folate deficiency; chronic kidney disease), RBCs being lost (bleeding, heavy menstrual bleeding), or RBCs being destroyed faster than they’re made (hemolysis, inherited hemoglobin disorders). The mission is to sort production vs. loss vs. destruction.
Red flags include: chest pain, shortness of breath at rest, syncope, rapid heart rate, or signs of active bleeding. Fever (≥100.4°F / 38.0°C) plus low Hct with infection may warrant urgent evaluation. A hemoglobin in the ~6–7 g/dL range (often corresponding to a markedly low Hct) in a hemodynamically stable adult is typically where transfusion may be considered—always individualized.
A practical rule of thumb is that if Hct is low, look for a story: iron intake, menstrual history, GI symptoms, chronic conditions, medications, and family history. That history steers which labs to add next.
Common Causes of Low Hct Levels
This section reviews the main conditions that drive Hct down.
- Iron deficiency anemia (IDA): Inadequate intake/absorption or chronic blood loss (e.g., heavy menses, GI bleeding).
- Anemia of chronic disease/inflammation: Complex iron handling; often coexists with IDA.
- Chronic kidney disease (CKD): Low erythropoietin (EPO) production blunts RBC synthesis.
- Vitamin B12 or folate deficiency: Macrocytosis with ineffective erythropoiesis.
- Pregnancy: Dilutional effect; IDA is common.
- Inherited hemoglobinopathies: Sickle cell disease, thalassemias.
- Bone marrow disorders: Aplastic anemia, myelodysplasia.
- Acute or occult bleeding: Trauma, GI sources, postpartum hemorrhage.
Diet matters. Heme iron (meat, seafood) is more bioavailable than non-heme iron (plants, fortified grains); vitamin C boosts non-heme iron absorption, while phytates and calcium can reduce it. A succinct, clinician-grade overview is available here ⧉.
Symptoms Associated with Low Hematocrit
Typical symptoms include fatigue, reduced exercise tolerance, dyspnea on exertion, palpitations, dizziness/lightheadedness, headache, cold intolerance, and pallor. Severe anemia can bring chest pain or shortness of breath at rest. In kids and teens, look for reduced attention, irritability, or pica (craving ice, clay). In pregnancy, low Hct is linked with prematurity and low birth weight if left untreated.
These symptoms are nonspecific—fatigue has many causes. That’s why CBC context is key: MCV, RDW, platelets, reticulocyte count, and iron studies sharpen the picture. As Reyus Mammadli, medical consultant, notes, “Symptoms are the smoke, not the fire—pair the story with ferritin and reticulocytes early to avoid chasing shadows.”
When to call the doctor depends on severity. If there’s active bleeding, chest pain, fainting, or rapidly worsening shortness of breath, seek urgent care. For new-onset fatigue plus tachycardia or very pale skin, sooner is better. For pregnancy, trimester-specific anemia thresholds apply (see below) ⧉.
Diagnostic Pathway: Tests That Follow Low Hct
Once low Hct is detected on CBC, the next step is to build a focused panel that answers why it is low. Below, tests are scored for practical “clinical utility” (1–10) and typical U.S. self-pay price examples; actual prices vary by lab and location.
| Test | What it tells you | Clinical utility (1–10) | Typical U.S. self-pay example |
|---|---|---|---|
| CBC with indices | Confirms anemia; MCV/MCH/RDW patterning (micro/macro/normocytic) | 10 | ~$26 at a national lab ⧉ |
| Reticulocyte count | Marrow response (production up or down) | 9 | ~$20–$60 depending on site |
| Ferritin, iron, TIBC, transferrin saturation | Iron stores and transport; diagnose IDA vs. anemia of chronic disease | 10 | Iron panel often ~$53; ferritin ~$59 ⧉ |
| Peripheral smear | Morphology (schistocytes, target cells, spherocytes) | 8 | Often bundled/variable |
| Vitamin B12 ± folate | Macrocytosis workup | 8 | Commonly ~$49–$82 |
| Hemoglobin electrophoresis | Detects hemoglobin variants (S, C, E); thalassemia patterns | 8 | ~$60–$150 typical consumer pricing |
| Genetic testing (thalassemia, etc.) | Confirms suspected inherited causes | 6–8 | Widely variable (~$100–$2,000) |
| Stool occult blood / colonoscopy | GI blood loss evaluation (age/risks guide) | 6–9 | Variable; procedure-level pricing |
Point-of-care (POC) hemoglobin/hematocrit devices can triage quickly in clinics and ERs; accuracy varies by model and setting ⧉. Modern analyzers (e.g., Sysmex XN series) add algorithmic flags for suspected iron deficiency or blasts; digital morphology analyzers can speed slide review—useful, especially when resources are stretched.
U.S. authorities define anemia in pregnancy as Hb <11 g/dL (≈Hct <33%) in 1st/3rd trimesters and Hb <10.5 g/dL (≈Hct <32%) in 2nd trimester ⧉. That nuance matters when deciding when to treat.
Expert tip — Reyus Mammadli: “Don’t skip the reticulocyte count. Low retics point you to production problems (iron/B12/folate, CKD). High retics push you to think bleeding or hemolysis. It’s a five-dollar test that saves five days.”
Treatment Options After Low Hematocrit Detection
Treatment depends on the cause while supporting oxygen delivery.
- Oral iron (ferrous sulfate 325 mg ≈ 65 mg elemental iron, typically once daily or every other day to improve absorption and tolerance). Pair with vitamin C–rich food; avoid calcium at the same time. Expect Hb/Hct to rise over 2–4 weeks, with ferritin repletion over 2–3 months.
- Intravenous (IV) iron for intolerance to oral iron, malabsorption, significant ongoing blood loss, or CKD. Common brands and typical dosing courses: Venofer® (iron sucrose; cumulative ~1,000 mg), Injectafer® (ferric carboxymaltose; 750 mg × 2 doses), Feraheme® (ferumoxytol; 510 mg × 2 doses). Hypersensitivity is uncommon but monitored; hypophosphatemia is a known risk with some formulations. Consult prescribing information for dosing and safety.
- Erythropoiesis-stimulating agents (ESAs) such as epoetin alfa (Epogen®/Procrit®) or darbepoetin alfa (Aranesp®) for CKD-related anemia when Hb is persistently low after iron optimization. Dosing is weight-based (e.g., epoetin 50–100 units/kg IV/SC weekly to biweekly). Target Hb is individualized; avoid overshooting.
- Transfusion of packed RBCs when symptomatic anemia is severe or there’s hemodynamic compromise. Contemporary guidelines favor a restrictive strategy in stable adults—often considering transfusion near Hb <7 g/dL—with clinical judgment on top ⧉. One unit is ~300 mL (~10 fl oz) and typically raises Hb by ~1 g/dL (Hct by ~3%).
- Address sources of loss (e.g., gynecologic or GI bleeding) and replete B12/folate if deficient.
With adequate iron, Hb usually increases ~1 g/dL every 2–3 weeks. Lack of response triggers a look for poor adherence, malabsorption, inflammation, or an alternative diagnosis.
Innovations in Managing Low Hematocrit
New approaches are changing care.
- CRISPR-based gene therapy for sickle cell disease: The FDA approved the first CRISPR therapy (CASGEVY™/exa-cel) for patients ≥12 years with recurrent vaso-occlusive crises. For applicable patients, restoring healthy hemoglobin production can normalize Hct and reduce crises ⧉.
- Next-gen hematology analyzers and AI flags: Automated analyzers increasingly provide iron-deficiency flags and digital morphology to speed up triage; studies continue to refine accuracy and workflow integration.
- HIF-PH inhibitors in CKD anemia: New oral agents (e.g., vadadustat) modulate the body’s hypoxia response to stimulate erythropoiesis—an emerging option in specific CKD populations, guided by safety data and labeling.
These innovations do not replace standard care. They expand the toolbox. Iron repletion, ESA use in CKD, and transfusion thresholds remain foundational; advanced therapies fit specific indications.
Real-Life Cases Across the U.S.
Examples from U.S. practice show how low Hct presents and is managed.
- Case 1 — Postpartum woman, 32, New York State: After a complicated delivery, Hct fell with symptomatic fatigue and dizziness. Oral iron caused intolerance; IV iron sucrose was given, with Hct and energy improving within weeks, aligning with data showing IV iron can correct postpartum anemia faster than oral iron in appropriate candidates.
- Case 2 — Man, 68, Southern California, CKD on dialysis: Persistent low Hct despite oral iron. Workup confirmed iron deficiency and low EPO production. IV iron was administered, then an ESA was started with careful Hb targets; transfusion was avoided as symptoms improved.
- Case 3 — Teen girl, 15, Midwest: Heavy menstrual bleeding and low dietary iron led to microcytic anemia (low Hct, low MCV, low ferritin). Education on heme vs. non-heme iron, every-other-day oral iron, and gynecologic follow-up corrected labs over two months.
(Details summarized from published U.S. reports and clinical guidance to preserve privacy; patterns mirror what large U.S. datasets describe.)
Prevention and Monitoring Strategies
Prevention is possible in many cases.
- Nutrition: Include iron-rich foods (heme sources like beef, lamb, poultry; non-heme sources like lentils, beans, spinach, iron-fortified cereals). Pair plant sources with vitamin C (citrus, berries) to enhance absorption. Limit tea/coffee with iron meals.
- Smart supplementation: For those at risk (menstruating teens, pregnancy, frequent blood donors), discuss periodic iron supplementation and timing (every other day can improve absorption).
- Chronic disease management: In CKD, coordinate iron repletion and ESA candidacy; in inflammatory conditions, treat the underlying process.
- Screening cadence: Annual CBC for at-risk groups is reasonable; more often if symptomatic or if you have conditions that commonly lower Hct.
- Athletes & altitude: Training plans at altitude (≥5,000 ft / ~1,524 m) and endurance sports can shift Hct; hydration and iron balance are key—don’t guess, test.
Quick do’s and don’ts: do follow up any unexpected low Hct with ferritin and reticulocytes. Do not self-transfuse supplements without a plan—iron overload is real. When in doubt, phone a friend (aka your clinician). As Americans say, “measure twice, cut once.”
Editorial Advice
From the editors (and a final word from Reyus Mammadli):
- Reyus Mammadli, medical consultant, recommends ordering ferritin + transferrin saturation + reticulocyte count at the first visit when Hct is low; this trims the diagnostic path by a week and nudges treatment sooner. He also suggests reviewing medications (e.g., proton pump inhibitors reducing iron absorption) before escalating to IV iron.
- Keep therapy cause-directed: oral iron for mild IDA with good tolerance; IV iron for intolerance/malabsorption/ongoing loss; ESAs for CKD per guideline; transfusion only when clinically necessary.
- Use restrictive transfusion thresholds in stable adults and aim for symptom relief + safe Hb targets, not a “perfect number.”
- Leverage modern analyzers/flags and POC tools to triage faster; confirm with ferritin and smear when the story is murky.
- Finally—track response. If Hct isn’t budging after 2–3 weeks, that’s your cue to reassess adherence, absorption, inflammation, or alternative diagnoses. Not a “set it and forget it” situation.