Fibrocystic breasts are composed of tissue that feels bumpy or rope-like in texture. Physicians call this nodular or glandular breast tissue.
It’s not at all uncommon to have fibrocystic breasts. Over half of women experience fibrocystic breast modifications eventually in their lives. In truth, doctor have actually stopped using the term “fibrocystic breast disease” and now simply describe “fibrocystic breasts” or “fibrocystic breast modifications” because having fibrocystic breasts isn’t really a disease. Breast modifications categorized as fibrocystic are considered regular.
Although many women with fibrocystic breasts don’t have symptoms, some women experience breast pain, tenderness and lumpiness — particularly in the upper, outer area of the breasts. Breast symptoms tend to be most annoying right before menstruation. Easy self-care steps can generally relieve discomfort related to fibrocystic breasts.
Symptoms and Signs of Fibrocystic Breasts
Signs and symptoms of fibrocystic breasts might consist of:
- Breast swellings or areas of thickening that tend to blend into the surrounding breast tissue
- Generalized breast pain or inflammation
- Breast lumps that vary in size with the menstruation
- Green or dark brown nonbloody nipple discharge that tends to leak without pressure or squeezing
- Breast modifications that are comparable in both breasts
- Month-to-month increase in breast pain or lumpiness from midcycle (ovulation) to just before your duration
Fibrocystic breast changes happen most often in women in their 20s to 50s. Seldom do postmenopausal women experience fibrocystic breast changes, unless they’re on hormone therapy.
When to see a doctor
The majority of fibrocystic breast changes are normal. However, make an appointment with your doctor if:
- You discover a new breast lump or area of prominent thickening
- You have specific areas of constant or getting worse breast pain
- Breast changes continue after your period
- Your doctor assessed a breast lump but now it appears to be bigger or otherwise altered
Causes of Fibrocystic Breast
- Growth of breast, consisting of lymph nodes, lobules and ducts
- Breast anatomy
The exact cause of fibrocystic breast changes isn’t known, however specialists believe that reproductive hormones — specifically estrogen — contribute.
Changing hormone levels during your menstruation can cause breast pain and areas of bumpy breast tissue that feel tender, sore and swollen. Fibrocystic breast changes have the tendency to be more irritating prior to your menstrual duration, and the pain and lumpiness tends to improve or reduce as soon as your menstrual period begins.
When examined under a microscope, fibrocystic breast tissue includes distinct elements such as:
- Fluid-filled round or oval sacs (cysts).
- A prominence of scar-like fibrous tissue (fibrosis).
- Overgrowth of cells (hyperplasia) lining the milk ducts or milk-producing tissues (lobules) of the breast.
- Enlarged breast lobules (adenosis).
Risk factors
Having fibrocystic breasts does not enhance your risk of breast cancer.
How Is Fibrocystic Breast Diagnosed?
Tests to evaluate your fibrocystic breast might include:
- Medical breast examination. Your doctor checks for unusual areas by aesthetically and manually examining your breasts and the lymph nodes located in your lower neck and underarm area. If your medical history and the clinical breast test indicate regular breast changes, you might not need added tests. If your doctor finds a brand-new lump and presumes fibrocystic modifications, you may come back a few weeks later, after your menstrual duration, to have another breast test. If the changes continue, you’ll likely need a mammogram or ultrasound.
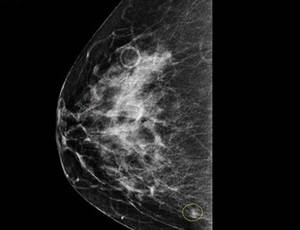
- Mammogram. If your doctor finds a breast swelling or prominent thickening in your breast tissue, you require a diagnostic mammogram — an X-ray examination that concentrates on a specific area of issue in your breast. The radiologist closely examines the area of issue when translating the mammogram.
- Ultrasound. An ultrasound uses sound waves to produce pictures of your breasts and is frequently carried out together with a mammogram. If you’re younger than age 30, you might have an ultrasound rather of a mammogram. Ultrasound is better for evaluating a more youthful woman’s dense breast tissue– tissue securely loaded with lobules, ducts and connective tissue (stroma). Ultrasound can likewise help your doctor compare fluid-filled cysts and solid masses.
- Fine-needle aspiration. For a breast swelling that feels a lot like a cyst, your doctor may attempt fine-needle goal to see if fluid can be withdrawn from the swelling. This useful procedure can be done in the workplace. A fine-needle goal may collapse the cyst and resolve pain.
- Breast biopsy. If a diagnostic mammogram and ultrasound are regular, however your doctor still has concerns about a breast lump, you may be described a breast specialist to figure out whether you require a surgical breast biopsy. A breast biopsy is a procedure to get rid of a little sample of breast tissue for tiny analysis. If a suspicious area is identified during an imaging examination, your radiologist might advise an ultrasound-guided breast biopsy or a sterotactic biopsy, which uses mammography to identify the precise area for the biopsy.
How Is Fibrocystic Breasts Treated?
If you don’t experience symptoms, or your symptoms are moderate, no treatment is required for fibrocystic breasts. Severe pain or big, painful cysts related to fibrocystic breasts might require treatment.
Treatment options for breast cysts include:
- Fine-needle aspiration. Your doctor uses a hair-thin needle to drain the fluid from the cyst. Eliminating fluid validates that the lump is a breast cyst and, in impact, collapses it, relieving associated discomfort.
- Surgical excision. Rarely, surgery might be had to get rid of a relentless cyst-like swelling that does not deal with after repeated goal and mindful monitoring or has functions that issue your doctor during a scientific examination.
Examples of treatment options for breast pain consist of:
- Non-prescription pain relievers, such as acetaminophen (Tylenol, others) or nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others) or prescription medication.
- Oral contraceptives, which lower the levels of cycle-related hormonal agents connected to fibrocystic breast modifications.
Alternative medicine for Fibrocystic Breasts
Vitamins and dietary supplements might decrease breast pain symptoms and intensity for some women. Ask your doctor if one of these might assist you– and inquire about doses and any possible side effects:
- Evening primrose oil. This supplement may alter the balance of fatty acids in your cells, which might decrease breast pain.
- Vitamin E. Early researches revealed a possible helpful impact of vitamin E on breast pain in premenstrual women who experience breast pain that fluctuates during the menstruation. In one research study, 200 global devices (IU) of vitamin E taken twice daily for two months improved symptoms in women with cyclic breast pain. There was no fringe benefit after 4 months.
For adults, pregnant women and breast-feeding women, the optimum dosage of vitamin E is 1,000 milligrams daily (or 1,500 IU).
If you try a supplement for breast pain, stop taking it if you don’t notice any enhancement in your breast pain after a couple of months. Try just one supplement at a time so that you can clearly identify which one helps alleviate the pain– or not.
Does Fibrocystic Breast Disease Affect Breastfeeding?
Fibrocystic breast disease influences nearly half of women of childbearing age. As we age, our breast tissue ends up being more thick and we might establish non-cancerous swellings or cysts, in addition to swelling, and tenderness or pain. Considering that numerous women are influenced, the American Cancer Society has actually suggested that healthcare suppliers use the term “fibrocystic changes,” instead of continuing to designate it as a disease. This condition falls back during pregnancy.
Breastfeeding delays the return of symptoms for some women. This condition should provide no particular issue for you while breastfeeding.
Can Fibrocystic Breast Cause Nipple Discharge?
Nipple discharge is another very common condition. A lot of women with nipple discharge are extremely concerned that they have cancer, however in fact, the majority of nipple discharge is what we refer to as “physiologic” — in other words, relevant to regular hormonal variations.
The discharge may be yellow, green, or brown — similar to cyst fluid. It might likewise be milky, especially in women who have actually had children.
Sometimes milky discharge is associated with elevations of a hormone called prolactin. Prolactin is normally produced during breast-feeding, but periodically developments in the pituitary gland (a small gland in the brain that produces a lot of the body’s hormones) can cause an elevated prolactin level. Generally, in the absence of a specific mass or irregularity on mammogram or ultrasound, no particular treatment for the discharge is shown. Periodically, an infection will be the cause of the discharge and will react to antibiotics.
Sometimes the discharge is clear and even bloody. This is typically due to a growth within a milk duct. Many times the growths are benign, but due to the capacity for cancer, anyone with bloody nipple discharge will be advised to have a biopsy to dismiss cancer.
Does Fibrocystic Breasts Cause Armpit Pain?
The degree to which women experience these symptoms differs substantially. Some women with fibrocystic breasts only experience mild breast pain and might not have the ability to feel any breast swellings when carrying out breast self-exams.
Other women with fibrocystic breasts might experience more severe breast pain or tenderness and may feel numerous swellings in their breasts. The majority of fibrocystic breast lumps are found in the upper, outer quadrant of the breasts (near the axilla, armpit, area), although these swellings can occur anywhere in the breasts.
Fibrocystic breast swellings tend to be smooth, rounded, and mobile (not connected to other breast tissue), though some fibrocystic tissue may have a thickened, irregular feel. The lumps or irregularities associated with fibrocystic breasts are frequently tender to touch and might enhance or decrease in size during the menstruation.
What About Caffeine While You Have Fibrocystic Breasts?
Removal of caffeine from the diet, is most likely the most popular alternative lifestyle method for fibrocystic breasts.
The first randomized study of a bigger number of women was performed by Virginia Ernster, M.D. 158 women removed all caffeine (coffee, tea, cola, chocolate) from their diets for 4 months, in addition to caffeinated medications. She found a substantial reduction in clinically palpable breast findings in the abstaining group compared with the control group, although the absolute modification in the breast lumps was rather small and thought about to be of little medical significance.
Several other studies have been done, leaving us with mixed reports: three research studies show no association in between methylxanthines and benign breast disease… and two studies show a connection with caffeine consumption.