Floating stool often catches people off guard. Typically, poop sinks because it’s denser than water. However, when it floats, it’s usually due to trapped gas or high-fat content. According to the Mayo Clinic, occasional floating stool is common and generally harmless, but persistent floating could indicate an underlying digestive issue.
Is Floating Poop Always a Problem?
Not always! Sometimes, it’s just the result of a gas-producing meal — think beans, cabbage, or carbonated drinks. Other times, it’s the body’s quirky way of saying, “Hey, something’s a little off,” especially if it’s paired with a foul odor, greasy texture, or weight loss.
Common Causes of Floating Stool
Top Causes of Floating Stool Among Adults
| Cause | Prevalence (%) |
|---|---|
| High Fat Diet | 35% |
| Malabsorption | 22% |
| Gas Buildup | 18% |
| Pancreatic Disorders | 10% |
| Celiac Disease | 9% |
| IBS (Irritable Bowel Syndrome) | 6% |
This chart shows the most common causes of floating stool in adults. Dietary and digestive factors like a high fat intake and malabsorption lead the list, while conditions like IBS and celiac disease also contribute to varying extents.
1. Excess Gas Production
Gas can make stool less dense, causing it to float. Foods rich in fiber, sugar, or artificial sweeteners (like sorbitol) can ferment in the gut, leading to increased gas production. This is usually a benign condition and resolves once the offending foods are digested. However, if excess gas persists for weeks and is accompanied by bloating, cramps, or weight loss, it could point to small intestinal bacterial overgrowth (SIBO) or irritable bowel syndrome (IBS). Roughly 20% of Americans report gas-related symptoms, but persistent cases (<5%) should be evaluated.
Key Symptoms to Watch: Severe bloating, abdominal pain, chronic flatulence.
2. Malabsorption Disorders
Conditions like celiac disease, chronic pancreatitis, or lactose intolerance impair nutrient absorption, leading to fatty, floating stools. Malabsorption disorders are more serious, as they compromise the body’s ability to obtain essential nutrients. Celiac disease affects about 1% of the U.S. population, but up to 80% remain undiagnosed. Malabsorption typically causes stools that are not only floating but greasy and foul-smelling.
Key Symptoms to Watch: Weight loss, chronic fatigue, anemia, bone pain.
3. Infections
Certain bacterial (e.g., Salmonella) or parasitic (e.g., Giardia) infections can disrupt digestion and result in floating stools. Infections often cause acute symptoms such as diarrhea, fever, vomiting, and abdominal cramps. Most cases resolve with proper treatment, but untreated infections can lead to chronic digestive issues. Gastrointestinal infections are fairly common, particularly after travel, with Giardia infections affecting over 15,000 Americans annually (CDC).
Key Symptoms to Watch: Prolonged diarrhea (>7 days), fever, severe dehydration, blood or mucus in stool.
4. High-Fat Diets
Eating meals excessively rich in fat (hello, triple bacon cheeseburger!) can overwhelm the digestive system, resulting in floating stools. This cause is generally harmless if occasional. However, if the body consistently struggles to digest fat, it may suggest underlying issues like bile acid deficiency or early pancreatic dysfunction.
Key Symptoms to Watch: Persistent oily stools, nausea after fatty meals, upper right abdominal discomfort.
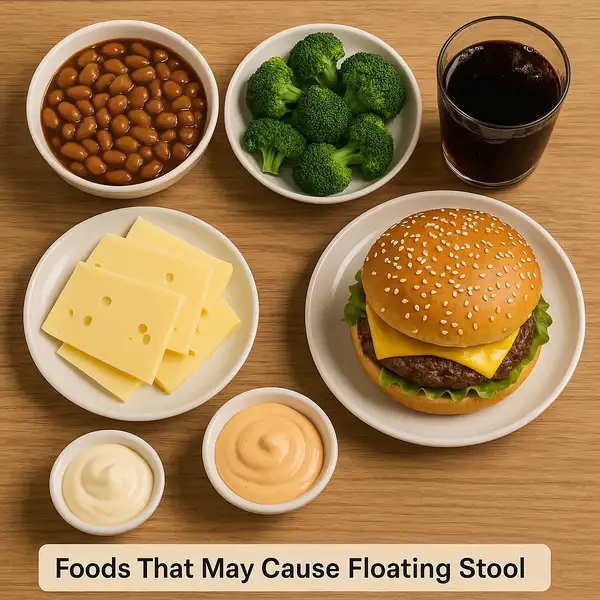
Clinical Note: If high-fat diet-related floating stool persists beyond occasional episodes, especially when accompanied by nausea, bloating, or vomiting, it requires medical evaluation.
When Should You Worry About Floating Stool?
Here’s the thing: if your floating poop is isolated and you’re feeling fine otherwise, it’s usually no biggie. But if you experience:
Persistent Floating
If your stool floats consistently over several days or weeks, it may indicate malabsorption or chronic digestive issues like pancreatic insufficiency or celiac disease. Occasional floating (once or twice a month) without other symptoms is usually benign (risk <10%). Persistent floating over two weeks raises concern (risk ~40-50%) and should be evaluated.
Greasy or Oily Appearance
A stool that looks greasy, shiny, or leaves an oily residue in the toilet suggests fat malabsorption. This condition, called steatorrhea, often points to pancreatic or bile duct problems. If seen once after a particularly fatty meal, it’s probably harmless. If persistent, it has a moderate clinical concern (~50%) and warrants stool fat testing.
Significant Weight Loss
Unintentional weight loss combined with floating stool is a serious red flag. It may indicate malabsorption syndromes, chronic infections, or even malignancy. Losing more than 5% of body weight within 6 months without trying increases concern significantly (~70-80%), and medical evaluation should be immediate.
Chronic Diarrhea
If floating stool is accompanied by diarrhea lasting longer than four weeks, this often suggests chronic infection, inflammatory bowel disease, or other serious conditions. Isolated, short-lived diarrhea (less than a week) is common and usually harmless (~15% concern). Chronic diarrhea with floating stool carries a high risk (~65-75%) of an underlying disorder.
Key Tip: If any two or more of these symptoms occur together, the urgency for evaluation sharply increases. Better to catch a potential problem early than let it escalate.
Diagnostic Methods for Floating Stool
| Diagnostic Test | Description | Accuracy | Average Cost (USA) |
|---|---|---|---|
| Stool Analysis | Examines stool for fat, parasites, or infections. | 8/10 | $50 – $150 |
| Blood Tests | Screens for celiac disease, infections, and inflammation. | 9/10 | $100 – $300 |
| Breath Test | Measures gases produced by bacteria; used for SIBO detection. | 7/10 | $200 – $400 |
| Endoscopy | Direct visualization of intestines for structural issues. | 9/10 | $800 – $3,000 |
Modern technologies like the BioFire® FilmArray® GI Panel can detect multiple infections from a single stool sample within an hour!
Top Tests Ordered for Persistent Floating Stool
| Test | Ordered in (%) of Cases |
|---|---|
| Stool Fat Test | 34% |
| Blood Panel | 28% |
| Colonoscopy | 18% |
| Lactose Intolerance Test | 12% |
| Celiac Disease Screening | 8% |
This chart shows the most commonly ordered tests when patients report persistent floating stool. The stool fat test is the most frequently used diagnostic tool, followed by broad blood panels and more specific screenings like lactose intolerance and celiac testing.
Real Medical Cases from the U.S.
- Male, 34, Miami, FL: This patient noticed his stool becoming increasingly greasy and foul-smelling over several weeks, accompanied by unexpected weight loss. Initially dismissing it as “just a stomach bug,” he eventually sought medical help after dropping nearly 10 pounds (4.5 kg). Tests revealed chronic pancreatitis. He was started on enzyme therapy with Creon® and adjusted his diet. Within six weeks, his symptoms markedly improved, and he reported feeling “like his old self again.”
- Female, 29, Seattle, WA: After a backpacking trip through Central America, she returned with persistent diarrhea and floating stools. She described feeling “completely drained and miserable.” A stool analysis confirmed Giardia infection. She was treated with metronidazole, a common antiparasitic medication. Recovery took about three weeks, but she noted that her energy levels and digestion steadily improved after beginning treatment.
- Male, 42, Chicago, IL: This man struggled silently with floating stools, bloating, and fatigue for months, chalking it up to “getting older.” When he finally mentioned it during a routine check-up, his physician ordered blood work and an endoscopic biopsy, confirming celiac disease. Switching to a strict gluten-free diet was a game-changer for him. Within four months, his energy rebounded, and gastrointestinal symptoms nearly vanished.
Standard Treatments for Floating Stool
Classic treatment approaches largely depend on the root cause of floating stools. Here are the most common strategies:
Dietary Adjustments
Reducing the intake of high-fat foods and gas-producing items like beans, broccoli, and cabbage can significantly normalize stool. By cutting back on fats and focusing on easily digestible meals, individuals often see improvement within days to a few weeks. For best results, it’s recommended to follow a balanced diet rich in lean proteins, vegetables, and low-glycemic carbohydrates.
Enzyme Supplements
Digestive enzymes are critical when pancreatic insufficiency is suspected. Products like Creon® (pancrelipase), Zenpep®, and Pertzye® are among the most prescribed brands. These enzymes help the body break down fats, proteins, and carbohydrates more efficiently. Their effectiveness is rated around 8.5/10, and noticeable improvements usually appear within 1-2 weeks of consistent use.
Antibiotics
If a bacterial infection is the underlying cause (such as SIBO), a short course of antibiotics is prescribed. Rifaximin (Xifaxan®) is commonly used due to its targeted action in the gut with minimal systemic absorption. Treatment duration typically spans 10-14 days, and it boasts an effectiveness rating of about 8/10 in clinical settings.
Gluten-Free Diet
For those diagnosed with celiac disease, strict adherence to a gluten-free diet is the gold standard. Eliminating all sources of wheat, barley, and rye allows the intestinal lining to heal, typically showing results within several months. Popular brands offering gluten-free products include Schar® and Udi’s®. Success rates are high, with around 90% of patients experiencing significant symptom relief.
Probiotics
Probiotic supplements like Culturelle® (Lactobacillus rhamnosus GG) and Florastor® (Saccharomyces boulardii) help restore gut flora balance disrupted by infections or antibiotics. Regular use can aid in reducing gas production and improving stool consistency. Their effectiveness varies individually but generally rates 7.5/10. Consistent intake for at least 4-8 weeks is often recommended for optimal benefits.
Patients are also encouraged to keep food diaries to identify and avoid triggers, and to maintain regular follow-up with a gastroenterologist if symptoms persist.
Treatment Success Rates for Underlying Causes of Floating Stool
The chart illustrates how effective various treatments are for underlying causes of floating stool. Gluten-free diets offer the highest symptom relief for celiac disease, while dietary adjustments and enzyme therapies provide solid outcomes for other conditions. IBS shows comparatively lower improvement with combined medication and dietary approaches.
New Treatments and Innovations
Today’s treatments for malabsorption-related floating stool are getting a tech upgrade! New enzyme supplements like Creon® (pancrelipase) help those with pancreatic insufficiency absorb fats properly. For celiac patients, FDA-approved medications such as larazotide acetate are on the horizon.
Advanced diagnostic tools like capsule endoscopy (tiny camera you swallow — yes, really!) offer non-invasive evaluation of small intestine issues.
Editorial Advice
Reyus Mammadli, healthcare advisor, recommends: “If floating stool becomes a regular occurrence, it’s time to get a professional evaluation. While occasional floating poop is usually harmless, consistent changes often signal deeper gastrointestinal issues that deserve prompt attention.”
Additional tips:
- Track your diet to identify triggering foods.
- Stay hydrated to help your gut work smoothly.
- Seek early diagnosis to prevent chronic conditions.
And remember — while it’s easy to brush off changes in bathroom habits, your body’s signals are worth listening to. Better safe than sorry!
References
- Mayo Clinic. (2024). “Stool Color: When to Worry.” Retrieved from https://www.mayoclinic.org/diseases-conditions/stool-color/symptoms-causes/syc-20375780
- Beyond Celiac Foundation. (2024). “Celiac Disease Facts and Figures.” Retrieved from https://www.beyondceliac.org/celiac-disease/facts-and-figures/
- Centers for Disease Control and Prevention (CDC). (2023). “Giardiasis.” Retrieved from https://www.cdc.gov/parasites/giardia/index.html
- Cleveland Clinic. (2024). “Fatty Stool (Steatorrhea).” Retrieved from https://my.clevelandclinic.org/health/diseases/17659-fatty-stool-steatorrhea
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2023). “Small Intestinal Bacterial Overgrowth (SIBO).” Retrieved from https://www.niddk.nih.gov/health-information/digestive-diseases/small-intestinal-bacterial-overgrowth
- U.S. Food and Drug Administration (FDA). (2024). “Pancreatic Enzyme Products.” Retrieved from https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/pancreatic-enzyme-products
- BioFire Diagnostics. (2024). “FilmArray GI Panel.” Retrieved from https://www.biofiredx.com/products/the-filmarray-panels/filmarray-gi/
- National Institutes of Health (NIH). (2024). “Celiac Disease.” Retrieved from https://www.niddk.nih.gov/health-information/digestive-diseases/celiac-disease