Hemoglobinopathies is the medical term for a group of blood conditions and illness that affect red blood cells. These disorders include both sickle cell disease (SCD) and thalassemia.
Hemoglobinopathies keeping an eye on ways discovering the number of people with these conditions and how having a hemoglobinopathy impacts their health, so that scientists and health care companies can ultimately improve the health of people with hemoglobinopathies. By studying the variety of individuals with hemoglobinopathies over time, we can find out if their numbers:
- Are rising, dropping, or remaining the exact same
- Differ by area of the country/region
- Vary amongst subgroups of individuals (by age, race, or ethnic culture).
Definition
Hemoglobinopathy is a type of genetic defect that leads to irregular structure of among the globin chains of the hemoglobin particle. Hemoglobinopathies are inherited single-gene conditions; for the most parts, they are inherited as autosomal co-dominant characteristics. Common hemoglobinopathies consist of sickle-cell disease. It is estimated that 7% of world’s population (420 million) are providers, with 60% of overall and 70% pathological remaining in Africa. Hemoglobinopathies are most common in populations from Africa, the Mediterranean basin and Southeast Asia.
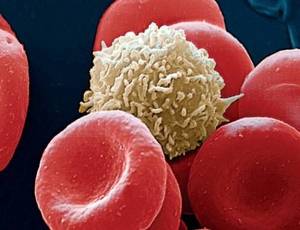
Hemoglobinopathies indicate structural problems in the globin proteins themselves. Thalassemias, on the other hand, generally lead to underproduction of normal globin proteins, typically through anomalies in regulatory genes. The 2 conditions might overlap, however, because some conditions which cause irregularities in globin proteins (hemoglobinopathy) likewise impact their production (thalassemia). Thus, some hemoglobinopathies are also thalassemias, but most are not.
Either hemoglobinopathy or thalassemia, or both, might cause anemia. Some widely known hemoglobin variations such as sickle-cell anemia and genetic dyserythropoietic anemia are accountable for illness, and are thought about hemoglobinopathies. However, numerous hemoglobin variations do not trigger pathology or anemia, and thus are often not classed as hemoglobinopathies, since they are not considered pathologies. Hemoglobin variants belong of the regular embryonic and fetal development, however may also be pathologic mutant forms of hemoglobin in a population, triggered by variations in genetics. Other variants trigger no detectable pathology, and are thus thought about non-pathological variations.
Normal Levels of Hemoglobin Types
A hemoglobin electrophoresis test doesn’t inform you about the quantity of hemoglobin in your blood — that’s carried out in a total blood count. The levels that a hemoglobin electrophoresis test describe are the percentages of the various kinds of hemoglobin that might be found in your blood. This is different in children and grownups:
In babies
Hemoglobin is mainly comprised of hemoglobin F in fetuses. Hemoglobin F still makes up the majority of hemoglobin in babies. It quickly decreases by the time your baby is a year old:
| Age | Hemoglobin F percentage |
| newborn | 60 to 80% |
| 1+ year | 1 to 2% |
In adults
The normal levels of the types of hemoglobin in adults are:
| Type of hemoglobin | Percentage |
| hemoglobin A | 95% to 98% |
| hemoglobin A2 | 2% to 3% |
| hemoglobin F | 1% to 2% |
| hemoglobin S | 0% |
| hemoglobin C | 0% |
Evolution
Some hemoglobinopathies (as well as related diseases like glucose-6-phosphate dehydrogenase deficiency) seem to have provided an evolutionary benefit, particularly to heterozygotes, in locations where malaria is endemic. Malaria parasites live inside red cell, however discreetly interrupt regular cellular function. In patients predisposed for quick clearance of red blood cells, this may lead to early damage of cells infected with the parasite and increased possibility of survival for the provider of the characteristic.
Hemoglobin functions:
- Transport of oxygen from the lungs to the tissues: This is because of the strange cooperation of the globin chains that allows the molecule to take in more oxygen where there is increased oxygen and to release oxygen in low concentration of oxygen.
- Transport of CO2 from the tissues to the lungs: The end item of tissue metabolism is acidic which increases hydrogen ions in service. The hydrogen ions integrate with bicarbonates to produce water and co2. The co2 is mop up by hemoglobin to favor this reversible reaction.
- Transportation of nitric oxide: Nitric oxide is a vasodilatator. This assists in the regulation of vascular reaction in times of stress as experienced throughout inflammation.
Pathology and natural structural abnormalities may lead to any of the following disease processes:
- Anemia due to minimized life expectancy of the red cells of lowered production of the cells e. g. hemoglobin S, C and E.
- Increased oxygen affinity: The red cell do not launch their oxygen material readily in hypoxic conditions. The bone marow for that reason needs to produce more red blood cells and there is polycythemia.
- Unstable hemoglobins: Red blood cells are quickly damaged under tension and hemolysis occurs with possible jaundice.
- Methemoglobinemia: The iron in the heme part of hemoglobin is quickly oxidised and this minimizes the capability of hemoglobin to bind oxygen. More deoxygenated hemoglobin are formed and the blood becomes cyanotic.