People who have hemorrhoids may experience pain when defecating. This unpleasant, painful sensation brings great discomfort to life. Here’s what we can advise you in this case.
It’s not likely that hemorrhoids are the source of your pain. Instead, the painful defecation you’re experiencing are a lot more likely to be due to a condition called an anal crack. Your health care company can confirm that with an examination. Anal fissures generally don’t disappear on their own, so it’s essential to have the condition effectively recognized and dealt with.
It’s typical for people to assume that their hemorrhoids are the reason for painful bowel movements. But, although hemorrhoids frequently trigger itching, irritation, level of sensitivity and other pain around the afflicted area, hemorrhoids hardly ever result in pain during a bowel movement.
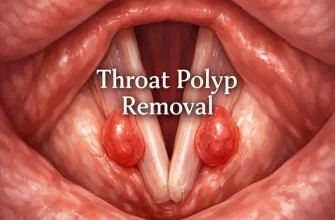
Anal cracks, nevertheless, are a frequent source of pain with bowel movements. These small tears occur in the skin around the rectum or in the thin tissue that lines the rectum, called the anoderm. An anal fissure might establish when you pass difficult or large stools throughout a defecation. Anal cracks generally trigger pain and bleeding with defecation.
When an anal crack occurs, the tear can expose the ring of muscle that holds your anus closed. This ring of muscle, called the internal sphincter muscle, lies underneath the anal skin and tissue. That direct exposure may set off spasms in the sphincter muscle. The spasms often activate more pain, and they likewise prevent the crack from healing. This establishes a vicious cycle of continuing pain.
A physical exam is usually all that’s needed to detect an anal fissure accurately. Treatment is completed in stages. Just how much treatment you require depends on how serious the crack is and how well it reacts to the preliminary treatment.
The initial step in treatment is to increase the quantity of fluid and fiber in your diet to make stools softer and easier to pass. That relieves pressure on the crack during bowel movements. Taking a bulking agent, such as Metamucil, Benefiber or Citrucel, can assist.
If the crack doesn’t recover within a number of weeks, the next step is to use a topical medication that’s applied to the skin to increase blood circulation to the fissure, promote recovery and assist the sphincter muscle unwind, thus reducing spasms. A topical kind of nitroglycerin or the calcium channel blocker nifedipine is frequently utilized for this purpose.
If the fissure persists despite these therapies, your health care provider might suggest an injection of botulinum toxin type A (Botox) into the internal sphincter muscle. That relieves spasms by incapacitating the muscle.
Lastly, if a crack still doesn’t heal with the other treatments, you might need surgery. A procedure called lateral internal sphincterotomy normally is used to treat chronic anal fissures. It involves cutting a little area of the internal sphincter muscle to decrease spasms and pain. Research has revealed that, for a fissure that doesn’t recover in time with medical treatment, surgery is frequently reliable. The procedure does, however, bring a small risk of causing brief incontinence to gas.
Make a visit to see your healthcare provider, and have your circumstance examined. If it is an anal fissure triggering pain throughout defecation, it’s essential to begin treatment as soon as possible to promote healing and prevent more damage.