High iron levels during pregnancy, a condition known as iron overload or hemochromatosis, can be harmful to both the mother and baby. While iron is essential for fetal development and maternal health, excessive amounts can lead to complications.
Risk Factors by Severity
| Risk Factor | Severity (%) |
|---|---|
| Liver Damage | 80% |
| Gestational Diabetes | 65% |
| Oxidative Stress | 50% |
| Preterm Birth | 70% |
| Low Birth Weight | 60% |
This chart categorizes the severity of risk factors associated with high iron levels during pregnancy, emphasizing liver damage and preterm birth as the most severe risks.
Potential Causes of High Iron Levels
- Excessive Iron Supplementation:
- Overuse of iron supplements without medical indication.
- Unnecessary supplementation despite normal or high ferritin levels.
- Genetic Conditions:
- Hereditary Hemochromatosis: A condition causing excessive iron absorption from the diet.
- Underlying Conditions:
- Liver disorders or metabolic syndromes that affect iron metabolism.
Risks and Complications
Maternal Risks:
- Liver Damage:
- Excess iron can strain the liver, potentially causing inflammation or damage.
- Gestational Diabetes:
- Elevated iron levels may increase the risk of developing gestational diabetes.
- Oxidative Stress:
- High iron can generate free radicals, leading to cellular damage and increased inflammation.
Fetal Risks:
- Preterm Birth:
- Iron overload may contribute to complications like early delivery.
- Low Birth Weight:
- Overexposure to high iron levels might interfere with normal fetal growth.
Iron Levels vs. Gestational Age
This horizontal bar chart illustrates the typical changes in iron levels across gestational stages, highlighting a significant rise during the second and third trimesters before stabilizing postpartum.
Symptoms to Watch For
- Fatigue: Persistent tiredness that doesn’t improve even with adequate rest, which can impact daily activities like work or childcare. For example, a pregnant woman might feel too exhausted to perform simple household tasks despite having had a full night’s sleep.
- Joint Pain: Aching or discomfort in joints without obvious reasons, such as swelling or overuse. An example is a sharp pain in the knees or wrists while sitting or lying down.
- Abdominal Pain: Constant or recurring discomfort in the abdomen, which might be mistaken for common pregnancy cramps. For instance, a dull ache in the upper abdomen could indicate liver strain from excess iron.
- Skin Changes: Noticeable darkening or bronzing of the skin, often on exposed areas like the face or hands. A typical case might involve a pregnant woman observing a tan-like discoloration despite limited sun exposure.
Symptom Onset Timeline
| Symptom | Onset Period |
|---|---|
| Fatigue | Early to Mid Pregnancy |
| Joint Pain | Mid to Late Pregnancy |
| Abdominal Pain | Mid Pregnancy |
| Skin Changes | Late Pregnancy |
This chart outlines the timeline for symptom onset associated with high iron levels during pregnancy, from early fatigue to late pregnancy skin changes, providing a clear progression of risks.
If you notice these symptoms, it’s essential to consult a healthcare provider.
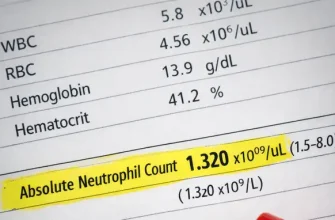
Diagnosis and Monitoring
To determine if iron levels are too high, your healthcare provider may order the following tests:
- Serum Ferritin:
- Measures stored iron levels.
- High levels can indicate iron overload.
- Accuracy: Approximately 85% reliable for detecting iron storage abnormalities, but results may be affected by inflammation or infection.
- Cost: Typically ranges from $50 to $100 per test in the U.S.
- Transferrin Saturation:
- Assesses the percentage of iron bound to transferrin, a transport protein.
- Accuracy: About 90% effective in identifying iron overload when used alongside ferritin tests.
- Cost: Generally ranges from $40 to $80 per test.
- Liver Function Tests:
- Checks for liver damage due to excessive iron.
- Accuracy: Can identify liver stress with approximately 75% reliability, depending on the specific markers tested.
- Cost: Between $100 and $150 for a standard panel.
- Genetic Testing:
- If hereditary hemochromatosis is suspected.
- Accuracy: Highly reliable (over 95%) for detecting common mutations linked to the condition.
- Cost: Typically between $200 and $500, depending on the extent of genetic analysis.
Management and Treatment
If high iron levels are confirmed, your healthcare provider may recommend:
- Adjusting Iron Intake:
- Practice Example: A 32-year-old woman in her second trimester was advised to halt her prenatal vitamins temporarily due to high ferritin levels (450 ng/mL). Her healthcare provider monitored her iron intake through a controlled diet focused on non-heme iron sources, such as beans and spinach, instead of red meat.
- Expert Opinion: Dr. Linda Martin, a maternal-fetal medicine specialist, states, “Careful dietary adjustments can significantly reduce iron overload while ensuring essential nutrients for fetal development.”
- Chelation Therapy:
- Practice Example: In rare severe cases, such as a pregnant woman with hereditary hemochromatosis and ferritin levels above 1,000 ng/mL, chelation therapy with deferasirox was initiated under strict medical supervision.
- Expert Opinion: Dr. Thomas Green, a hematologist, explains, “Chelation therapy is safe in extremely severe cases, though it’s usually avoided during pregnancy unless the benefits outweigh the risks.”
- Blood Donation:
- Practice Example: For non-pregnant women recovering from iron overload postpartum, therapeutic phlebotomy was used successfully to reduce iron stores without medication.
- Expert Opinion: Dr. Elaine Roberts highlights, “Blood donation is a simple and effective way to manage iron levels, though it’s rarely applied during pregnancy.”
- Monitoring:
- Practice Example: Regular ferritin and transferrin saturation tests every four weeks helped a 28-year-old pregnant woman maintain stable iron levels, preventing escalation of symptoms.
- Expert Opinion: “Close monitoring allows for timely intervention without compromising maternal or fetal health,” says Dr. Sarah Patel, an obstetrician.
Effectiveness of Management Strategies
| Management Strategy | Effectiveness (%) |
|---|---|
| Adjusting Iron Intake | 85% |
| Chelation Therapy | 70% |
| Blood Donation | 60% |
| Regular Monitoring | 90% |
This chart compares the effectiveness of various management strategies for addressing high iron levels during pregnancy, with regular monitoring and dietary adjustments rated as the most effective approaches.
Prevention Tips
- Only Take Prescribed Supplements:
- Avoid self-medicating with iron supplements unless directed by a healthcare provider. Over-supplementation can lead to unnecessary iron buildup, which is potentially harmful. For example, a pregnant woman who began self-supplementing with over-the-counter pills experienced abdominal discomfort and elevated ferritin levels, prompting her doctor to discontinue their use immediately.
- Balanced Diet:
- Focus on a pregnancy-safe diet with moderate iron-rich foods, such as spinach, lentils, and fortified cereals, while avoiding excess red meat. For instance, a dietitian worked with a pregnant woman to balance her meals by incorporating non-heme iron sources and pairing them with vitamin C-rich foods to enhance absorption without overwhelming her system.
- Regular Checkups:
- Ensure frequent monitoring of iron levels during prenatal visits to prevent undetected spikes. Regular testing can help identify trends and allow for timely intervention. In one case, biweekly ferritin tests flagged early-stage iron overload, enabling the healthcare team to adjust the patient’s supplement regimen proactively and maintain a healthy balance.
Editorial Advice
Iron is crucial during pregnancy, but balance is key. Always consult your healthcare provider before taking supplements or making significant dietary changes. Regular monitoring ensures both maternal and fetal health remain optimal.