Idiopathic Intracranial Hypertension (IIH), sometimes known as pseudotumor cerebri, is a neurological condition characterized by increased pressure within the skull without any apparent cause. IIH can present significant challenges to patients and medical professionals alike, given the complex interplay of symptoms and the relatively obscure nature of its origins.
What is Idiopathic Intracranial Hypertension?
Idiopathic Intracranial Hypertension involves an abnormal increase in cerebrospinal fluid (CSF) pressure around the brain, which can lead to symptoms similar to those of a brain tumor—hence the term pseudotumor cerebri. The condition is termed “idiopathic” because its exact cause is unknown, although some risk factors have been identified.
| Key Facts About IIH | Statistics |
|---|---|
| Incidence Rate | Approximately 1 per 100,000 people |
| Most Commonly Affects | Women of childbearing age |
| Gender Disparity | Women are 8 times more likely |
| BMI Association | High BMI increases risk significantly |
Symptoms and Signs
The symptoms of IIH are often debilitating, which can impact a patient’s quality of life significantly. The most common symptoms include:
- Headaches: Often described as severe, throbbing, and frequently occurring, these headaches are usually worse in the morning or when lying down. Some patients report that headaches worsen with physical activity.
- Vision Problems: Blurred or double vision is a common complaint, with some patients experiencing brief visual loss episodes or seeing flashes of light. Papilledema, or swelling of the optic nerve, is often detected during eye examinations.
- Tinnitus: Pulsatile tinnitus, where patients hear a “whooshing” noise in their ears in sync with their heartbeat, is another frequent symptom.
- Neck and Shoulder Pain: Pressure around the base of the skull often radiates to the neck and shoulders, causing discomfort.
Who is at Risk?
Idiopathic Intracranial Hypertension most commonly affects women between the ages of 20 and 50, particularly those who are overweight or have recently experienced weight gain. In fact, obesity is considered a major risk factor for IIH. A recent study found that nearly 90% of those diagnosed with IIH had a body mass index (BMI) greater than 30.
Interestingly, the incidence rate of IIH is increasing alongside the global rise in obesity rates, indicating a clear connection between lifestyle factors and the condition. While women are most frequently affected, men with higher BMIs are also at risk, though less commonly than women.
Statistics of Idiopathic Intracranial Hypertension (IIH) Incidence
Diagnostic Process
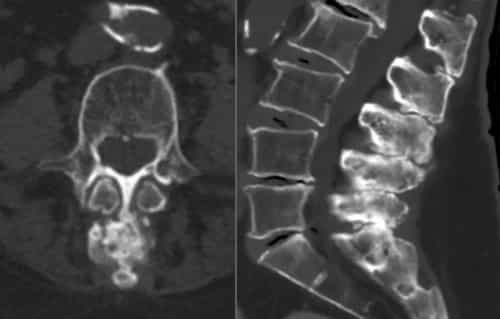
Diagnosis of IIH typically involves a series of tests aimed at excluding other possible causes of increased intracranial pressure, such as a brain tumor or other structural abnormalities.
| Diagnostic Test | Average Cost (USD) | Purpose |
|---|---|---|
| Ophthalmic Examination | $150 – $250 | To detect papilledema |
| Lumbar Puncture (Spinal Tap) | $800 – $1,500 | To measure CSF pressure |
| Brain MRI | $1,000 – $5,000 | To rule out structural abnormalities |
A lumbar puncture, also known as a spinal tap, is the definitive test for IIH, as it directly measures the pressure of cerebrospinal fluid. This test, while informative, is invasive and can cause discomfort, making it an option used only after other potential causes have been excluded.
Treatment Options for IIH
The treatment for IIH generally involves reducing intracranial pressure and alleviating symptoms. Treatments vary based on the severity of the symptoms and the patient’s specific circumstances.
- Weight Management: Weight loss is one of the most effective treatments for IIH in overweight individuals. Studies indicate that even a modest weight reduction of 5-10% can lead to symptom relief in many patients.
- Medications: The diuretic acetazolamide is commonly prescribed to decrease the production of cerebrospinal fluid, thereby reducing pressure. The cost of acetazolamide can range from $30 to $80 for a monthly supply, depending on the dosage.
- Surgical Options: In severe cases where vision is threatened or medications are ineffective, surgical interventions may be considered. Options include shunt surgery, which involves placing a tube to drain excess CSF, or optic nerve sheath fenestration to relieve pressure on the optic nerves.
| Treatment Type | Average Cost (USD) | Use Case |
|---|---|---|
| Acetazolamide (monthly) | $30 – $80 | To reduce CSF production |
| Shunt Surgery | $15,000 – $25,000 | For severe cases with vision risk |
| Optic Nerve Fenestration | $10,000 – $20,000 | To relieve pressure on optic nerves |
Real-World Example: Living with IIH
Consider a 35-year-old woman diagnosed with IIH after experiencing months of severe headaches and vision disturbances. Her ophthalmologist noted papilledema during a routine eye exam, prompting further investigation. An MRI ruled out other conditions, and a lumbar puncture confirmed increased CSF pressure. She was placed on acetazolamide and was advised to lose weight. After a 7% reduction in her body weight, she experienced significant relief from her symptoms, underscoring the importance of weight management in managing IIH.
Advice from Our Editorial Team
If you are experiencing persistent headaches, visual disturbances, or any of the symptoms listed above, it is essential to seek medical evaluation as soon as possible. IIH, while challenging, can often be managed effectively with the right combination of lifestyle modifications and medical treatment. For those at risk—particularly women with a higher BMI—consider working with a healthcare professional to develop a sustainable weight management plan. Early intervention is key to preventing the long-term effects of elevated intracranial pressure, including potential vision loss.