Ever found yourself wondering if that scary blood clot you were diagnosed with has finally packed its bags and left? You’re not alone. Millions of people in the U.S. face the same question every year — and figuring it out isn’t as simple as waiting for the pain to disappear. The good news? Modern medicine offers accurate ways to know if your clot is truly gone, and it’s not all doom and gloom.
Understanding Blood Clots — When the Body’s Defense Turns Risky
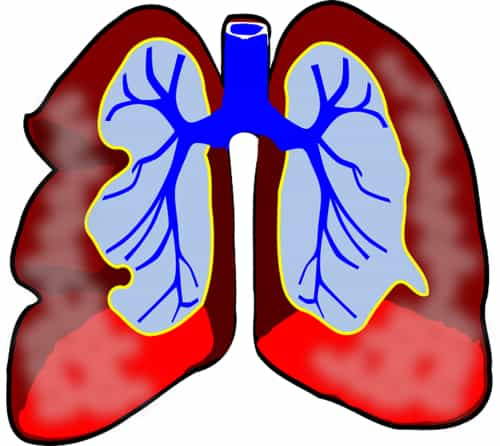
A blood clot (also called a thrombus) is the body’s natural way to stop bleeding. But when that mechanism misfires — say, inside a deep vein — it can spell trouble. Deep Vein Thrombosis (DVT) typically forms in the legs and can become dangerous if it travels to the lungs, causing a pulmonary embolism.
Risk factors include long flights, surgeries, pregnancy, aging, obesity, and certain medications. According to CDC estimates, nearly 900,000 Americans experience DVT or pulmonary embolism each year ⧉.
Think of it like this: your blood clot is a traffic jam in your bloodstream. Once the congestion clears — either naturally or through treatment — blood flow resumes smoothly, and symptoms begin to fade.
Typical Symptoms of a Blood Clot — And When They Start to Fade
When a blood clot forms, your body often sends clear warning signs — though they can differ from person to person. The most common are swelling, warmth, redness, tenderness, and localized pain, especially in the calf or thigh. The pain is often described as a deep ache or pressure, not unlike the soreness after an intense workout — except it doesn’t go away with rest.
Imagine your leg as a garden hose. When water flows freely, the hose is soft and flexible. But if there’s a kink in the middle, pressure builds, the hose stiffens, and the water slows. That’s what a clot does inside your veins — it blocks smooth circulation, creating a tight, heavy feeling that worsens when you stand or walk.
As the clot begins to dissolve and blood flow improves, the symptoms gradually fade. The swelling goes down, warmth subsides, and the leg starts to feel lighter. However, this improvement doesn’t always mean the clot is gone — only that the inflammation has eased.
Some people also experience skin discoloration — a reddish or bluish tint — that may take months to normalize. Persistent tenderness or mild swelling can remain for a while, a condition known as post-thrombotic syndrome (PTS). It occurs in about 30–40% of DVT patients ⧉.
Real-life examples highlight how deceptive symptoms can be. A 52-year-old woman from Texas reported that her leg pain was nearly gone after two months of treatment, but a follow-up ultrasound revealed a residual clot. Meanwhile, a 41-year-old man from Oregon said his calf felt normal again — and his imaging confirmed complete recovery. The takeaway? Relief is encouraging, but confirmation through testing is essential.
How Long Does It Take for a Blood Clot to Go Away?
There’s no universal answer. Small clots can resolve within a few weeks, while larger ones may take three months or longer. A study from the American Heart Association found that most patients see significant improvement within 90 days ⧉. Factors such as age, mobility, hydration, and medication adherence play major roles.
Reyus Mammadli, a medical consultant, notes that the key determinant is how consistent patients are with their anticoagulant therapy and follow-up care. “Skipping doses or stopping too early can reset your progress completely,” he explains.
Diagnostic Tests — How to Confirm If a Blood Clot Is Gone
Ultrasound (duplex scanning) is the gold standard for checking if a blood clot remains. It’s painless, non-invasive, and about 90% accurate. Average cost: $150–$300. It shows whether blood flow has normalized and if any clot fragments persist.
Blood tests, like the D-dimer, can help too. This test measures clot breakdown products — low levels usually mean the clot is gone. Accuracy: 8/10. However, factors like infection or inflammation can skew results.
Advanced imaging such as MRI or CT venography with contrast offers near-perfect accuracy (9.5/10). Hospitals often use systems like Philips Ingenia or Siemens Magnetom for high-resolution vascular imaging ⧉. These tests are more expensive ($500–$1,200) but provide detailed insights into deep or complex clots.
Treatment Innovations — From Anticoagulants to Smart Monitoring
Modern anticoagulants such as Eliquis, Xarelto, and Pradaxa have revolutionized blood clot management. Unlike older drugs, they don’t require constant blood tests or strict diet restrictions. They work by preventing new clots while allowing old ones to dissolve naturally.
Emerging technologies now include portable INR monitors and telemedicine-based tracking apps ⧉. According to Reyus Mammadli, these innovations empower patients to monitor their progress from home and catch issues early. “We’re moving toward proactive clot management rather than reactive care,” he emphasizes.
Real-Life Recovery Stories from the U.S.
A 67-year-old man from Florida developed a DVT after hip surgery. After three months on Xarelto and wearing compression stockings, his swelling subsided completely. Ultrasound confirmed full resolution.
Meanwhile, a 34-year-old woman from Illinois — a long-haul flight attendant — faced recurring DVTs. Through consistent use of Eliquis and remote monitoring, she achieved full recovery and returned to work without restrictions. These stories remind us that persistence and follow-up make all the difference.
When to See a Doctor — Don’t Guess, Get Checked
Even if you feel better, never assume the clot has vanished. Red flags include sudden shortness of breath, chest pain, dizziness, or new leg swelling. These could signal another clot or embolism. Doctors recommend follow-up imaging within 3–6 months post-diagnosis ⧉.
Reyus Mammadli advises patients to treat clot recovery like a marathon, not a sprint. “Your symptoms are just one clue — your scan tells the truth.”
Prevention and Lifestyle After a Blood Clot
Once the clot clears, prevention becomes the focus. Staying hydrated (8–10 glasses daily or about 2–2.5 liters / roughly 68–85 ounces), maintaining a balanced diet rich in omega-3 and vitamin E, and regular movement (walking 30 minutes daily) all help prevent recurrence.
Compression stockings (20–30 mmHg or 2.6–4.0 psi) support vein health and reduce swelling. Doctors also suggest avoiding long periods of sitting — if you work at a desk, get up every hour. The American College of Cardiology reports that lifestyle changes reduce recurrence risk by up to 60% ⧉.
Editorial Advice
According to Reyus Mammadli, patients should never judge recovery by symptom relief alone. “A clot can partially dissolve but still pose risks if fragments remain,” he notes. Always confirm through imaging before stopping medication.
His advice: schedule routine check-ups, follow your prescribed anticoagulant plan, and stay alert for warning signs. With modern diagnostics and smart monitoring, most patients today achieve full recovery and return to normal life — minus the fear.