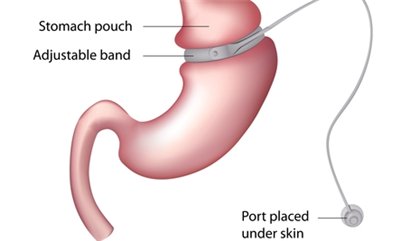
Laparoscopic gastric banding (LGB) is a minimally invasive bariatric surgery designed to help individuals with severe obesity achieve significant weight loss. This procedure involves placing an adjustable silicone band around the upper part of the stomach, creating a small pouch that limits food intake.
Average Weight Loss After Laparoscopic Gastric Banding (lbs)
The chart illustrates the average weight loss over time following laparoscopic gastric banding. The data shows significant weight reduction within the first few years, with a gradual plateauing effect over time.
Unlike gastric bypass or sleeve gastrectomy, LGB does not involve cutting or stapling the stomach, making it a reversible and adjustable option for weight management.
Who Is a Candidate for Laparoscopic Gastric Banding?
LGB is typically recommended for individuals who:
- Have a Body Mass Index (BMI) of 40 or higher, or BMI of 30-39.9 with obesity-related health conditions such as diabetes or hypertension. Obesity-related health conditions can include sleep apnea, fatty liver disease, and heart disease, all of which may significantly impact daily life and overall well-being.
- Have struggled with traditional weight loss methods (diet, exercise, medication) without long-term success. Many candidates have tried multiple diet plans, fitness programs, and even weight-loss medications but found only temporary or minimal results, leading to frustration and health deterioration over time.
- Are committed to making permanent lifestyle changes to support weight loss. This includes adhering to a structured post-surgery diet, attending regular follow-up visits for band adjustments, and incorporating physical activity into daily routines. It often takes several months to a year of consultation, medical evaluation, and psychological readiness assessments before a patient can proceed with surgery.
Prevalence of Obesity in the U.S. by Year (%)
The chart illustrates the rising prevalence of obesity in the U.S. over the years. The steady increase highlights the growing concern regarding obesity-related health issues.
How the Procedure Works
- Preparation: The patient undergoes preoperative testing, including blood work and imaging, to ensure suitability for surgery. Think of this as a car inspection before a long road trip—ensuring everything is in good shape before taking the next step.
- Surgery: Using laparoscopic techniques, a surgeon makes small incisions in the abdomen and inserts a camera and surgical instruments. This is similar to using a tiny telescope to work with precision instead of making a large cut, leading to a faster recovery.
- Placement of the Band: A silicone band is wrapped around the upper stomach, forming a small pouch. Imagine cinching a belt around a balloon to create a smaller compartment—this helps limit food intake without removing any part of the stomach.
- Adjustability: A tube connected to the band allows for fluid adjustments, controlling the tightness of the band to regulate food intake. This is much like tightening or loosening a wristwatch strap to ensure comfort and effectiveness.
- Recovery: Most patients return home the same day or within 24 hours, with a full recovery expected within two to four weeks. Think of it as taking a short break after a minor repair before getting back to daily life.
Accuracy and Cost of Diagnosis
| Diagnostic Method | Description | Accuracy | Estimated Cost (U.S.) |
|---|---|---|---|
| BMI Calculation | Determines obesity level | 9/10 | Free |
| Blood Tests | Checks for metabolic conditions | 8/10 | $50-$300 |
| Endoscopy | Examines stomach health | 9/10 | $1,000-$2,500 |
| Psychological Evaluation | Assesses mental readiness | 8/10 | $100-$500 |
Benefits of Laparoscopic Gastric Banding
- Minimally Invasive: Shorter recovery time compared to traditional bariatric surgeries, usually allowing patients to resume normal activities within a few days.
- Reversible & Adjustable: The band can be tightened, loosened, or removed if needed, making it a flexible solution for weight loss management over the long term.
- Gradual Weight Loss: Helps patients lose weight steadily, reducing risks of rapid weight loss complications such as gallstones, muscle loss, and excessive skin sagging.
- Lower Risk of Nutritional Deficiencies: Unlike gastric bypass, LGB does not interfere with nutrient absorption, allowing patients to maintain better overall nutrition.
- Less Surgical Risk: Because the procedure does not require cutting or stapling of the stomach, there is a lower risk of serious complications such as leaks or internal bleeding.
- Fewer Lifestyle Restrictions: Patients can still consume a variety of foods, though in smaller portions, and the band can be adjusted over time to optimize weight loss.
- Potential for Long-Term Maintenance: If properly adjusted and supported by behavioral changes, LGB can help maintain weight loss for many years, reducing the likelihood of weight regain.
Cost of Bariatric Surgeries in the U.S. (USD)
| Surgery Type | Cost (USD) |
|---|---|
| Gastric Bypass | $23,000 |
| Sleeve Gastrectomy | $19,000 |
| Laparoscopic Gastric Banding | $14,000 |
| Duodenal Switch | $25,000 |
This chart compares the costs of different bariatric surgeries in the U.S. Duodenal Switch is the most expensive, while Laparoscopic Gastric Banding is the most affordable option.
Risks and Potential Complications
While LGB is generally safe, some potential risks include:
- Band slippage or erosion requiring surgical correction, which may involve repositioning or removing the band if complications persist.
- Infection at the port site, potentially leading to abscess formation that requires antibiotic treatment or minor surgical intervention.
- Acid reflux or difficulty swallowing due to excessive band tightening, which can often be alleviated by adjusting the band’s fluid levels.
- Insufficient weight loss if dietary recommendations are not followed, often necessitating additional nutritional counseling and behavioral support to ensure long-term success.
- Possible esophageal dilation over time if the band is too tight, which may result in discomfort and require band loosening or removal.
- Risk of food intolerance or difficulty in digesting certain foods, leading to nausea or vomiting, which may necessitate dietary modifications and careful meal planning.
- Potential scarring or adhesions at the surgical site, which can sometimes cause long-term discomfort or require additional interventions.
- Port malfunction, where the access device used to adjust the band fails, necessitating surgical correction to replace or repair the component.
Patient Satisfaction Rate After Weight Loss Surgery (%)
| Surgery Type | Satisfaction Rate (%) |
|---|---|
| Gastric Bypass | 85% |
| Sleeve Gastrectomy | 80% |
| Laparoscopic Gastric Banding | 72% |
| Duodenal Switch | 88% |
This chart compares patient satisfaction rates for different types of weight loss surgeries. Duodenal Switch has the highest satisfaction rate, while Laparoscopic Gastric Banding has the lowest.
Medical Case: Real-Life Success Story
A 42-year-old woman from Texas with a BMI of 42 underwent laparoscopic gastric banding after years of struggling with obesity-related hypertension and joint pain. Within 18 months, she lost 85 pounds and significantly reduced her medication dependency. Her doctor adjusted the band three times over this period, ensuring a steady weight loss while maintaining nutritional balance.
Editorial Advice
Reyus Mammadli, healthcare advisor, recommends laparoscopic gastric banding as a viable option for individuals seeking a customizable, reversible approach to weight loss. However, success largely depends on patient commitment to dietary changes and follow-up care. It is essential to work with a qualified bariatric team and undergo regular adjustments to achieve optimal results.
For those considering bariatric surgery, consulting with a board-certified specialist is the first step toward a healthier future.
Reoperation Rates for Laparoscopic Gastric Banding (%)
| Time Period | Reoperation Rate (%) |
|---|---|
| 1 year | 5% |
| 2 years | 8% |
| 3 years | 12% |
| 5 years | 20% |
| 10 years | 30% |
This chart displays reoperation rates for laparoscopic gastric banding over different time periods, indicating an increasing likelihood of reoperation as time progresses.
References
- Mayo Clinic. (n.d.). Laparoscopic Adjustable Gastric Banding. https://www.mayoclinic.org/tests-procedures/gastric-banding/about/pac-20385192
- NIDDK. (n.d.). Bariatric Surgery Procedures. https://www.niddk.nih.gov/health-information/weight-management/bariatric-surgery/types
- ASMBS. (n.d.). Gastric Banding. https://asmbs.org/patients/bariatric-surgery-procedures#gastric-band
- WebMD. (n.d.). Laparoscopic Gastric Banding Surgery. https://www.webmd.com/diet/obesity/gastric-banding-surgery-for-weight-loss
- PubMed. (n.d.). Studies on Laparoscopic Gastric Banding. https://pubmed.ncbi.nlm.nih.gov/