Eye floaters are those tiny spots, specks, flecks and “cobwebs” that wander aimlessly around in your visual field. While annoying, normal eye floaters and spots are very common and normally aren’t cause for alarm.
Floaters and areas typically appear when small pieces of the eye’s gel-like vitreous break loose within the inner back part of the eye.
When we are born and throughout our youth, the vitreous has a gel-like consistency. But as we age, the vitreous begins to liquify and melt to produce a watery center.
Some undissolved gel particles sometimes will float around in the more liquid center of the vitreous. These particles can handle numerous shapes and sizes to become exactly what we describe as “eye floaters.”
You’ll see that these types of areas and eye floaters are specifically pronounced when you peer at a brilliant, clear sky or a white computer system screen. However you can’t in fact see small bits of debris floating loose within your eye. Instead, shadows from these floaters are cast on the retina as light go through the eye, and those shadows are what you see.
You’ll also notice that these specks never seem to stay still when you attempt to focus on them. Floaters and spots move when your eye steps, producing the impression that they are “drifting.”
When Are Eye Floaters and Flashes a Medical Emergency?
If you see a shower of floaters and areas, often accompanied by light flashes, you ought to seek medical interest immediately.
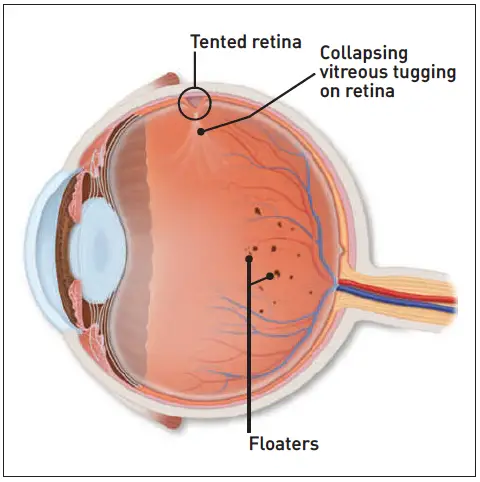
The unexpected look of these symptoms could suggest that the vitreous is pulling away from your retina or that the retina itself is ending up being dislodged from the inner back of the eye that contains blood, nutrients and oxygen important to healthy function. When the retina is torn, vitreous can get into the opening and push out the retina – resulting in a detachment.
A research reported in the Journal of the American Medical Association in 2009 discovered that sudden presence of eye floaters and flashes suggests that a person in seven people with these symptoms will have a retinal tear or detachment.
And approximately 50 percent of people with a retinal tear will have a subsequent detachment.
In cases of retinal tear or detachment, action should be taken as quickly as possible so that an eye specialist can reattach the retina and bring back function before vision is lost completely.
Posterior vitreous detachments (PVDs) are much more typical than retinal detachments and typically are not an emergency situation even when floaters appear suddenly. But some vitreous detachments also can damage the retina by pulling on it, causing a tear or detachment.
Light flashes known as photopsia can take place when your retina receives non-visual (mechanical) stimulation, which can occur when it is being tugged, torn or detached.
What Causes Eye Floaters and Spots?
As mentioned above, posterior vitreous detachments or PVDs prevail causes of vitreous floaters. Far less frequently, these symptoms can be connected with retinal tears or detachments that may be linked to PVDs.
However what leads to vitreous detachments in the very first location?
As the vitreous gel fills the inside of the back of the eye, it presses versus and really connects to the retina. In time, the vitreous ends up being more melted in the center. This in some cases indicates that the main, more watery vitreous can not support the weight of the heavier, more peripheral vitreous gel.
Vitreous gel then collapses into the central, liquefied vitreous. While this occurs, the peripheral vitreous detaches from the inner back of the eye where the retina lies.
Eye floaters resulting from a vitreous detachment are then concentrated in the more liquid vitreous discovered in the indoor center of the eye.
More than half of all individuals by the time they are 80 will have had a vitreous detachment. * If you are amongst the 40 percent of individuals with PVDs who also experience light flashes, then you have about a 15 percent opportunity of also developing a retinal tear.
Light flashes during this process suggest that traction is being applied to your retina while the PVD happens. When the vitreous lastly removes and pressure on the retina is reduced, the light flashes ought to slowly diminish.
What Causes Eye Flashes?
Normally, light entering your eye stimulates the retina. This produces an electrical impulse, which the optic nerve sends to the brain. The brain then translates this impulse as light or some type of image.
If the retina is mechanically promoted (physically touched), a similar electrical impulse is sent out to the brain. This impulse is then interpreted as a “flicker” of light.
When the retina is tugged, torn or removed from the back of the eye, a flash or flicker of light commonly is seen. Depending upon the level of the tear or detachment, these flashes of light might be brief or continue indefinitely until the retina is fixed.
Flashes (photopsia) also may take place after a blow to the head, often called “seeing stars.”
Some individuals experience flashes of light that look like rugged lines or “heat waves” in both eyes, typically long lasting 10-20 minutes. These types of flashes are usually triggered by a spasm of capillary in the brain, which is called a migraine.
If a headache follows the flashes, it is called a migraine headache. Nevertheless, jagged lines or “heat waves” can take place without a headache. In this case, the light flashes are called an ophthalmic migraine, or a migraine without a headache.
Photopsia likewise can be a symptom of digitalis toxicity, which can happen specifically in older individuals who take digitalis or associated drugs for heart problems.
Other Conditions Associated With Eye Floaters and Flashes
Researches show that bleeding (vitreous hemorrhage) accompanying a PVD means phenomenal traction has actually taken place, which increases the possibility of a retinal tear or detachment. Traction applied on the retina throughout a PVD likewise can cause advancement of conditions such as macular holes or puckers.
Vitreous detachments with accompanying eye floaters likewise might occur in situations such as:
- Inflammation in the eye’s interior.
- Nearsightedness.
- Cataract surgery.
- YAG laser eye surgery.
- Diabetes (diabetic vitreopathy).
- CMV retinitis.
Inflammation connected with many conditions such as eye infections can trigger the vitreous to liquefy, causing a PVD.
When you are nearsighted, your eye’s elongated shape also can increase the possibility of a PVD and accompanying traction on the retina. In reality, nearsighted people are more likely to have PVDs at a younger age.
PVDs are typical following cataract surgery and a follow-up procedure called a YAG laser capsulotomy. The laser treats a cataract surgery issue where cloudiness develops in the pill underlying the synthetic lens (IOL). Eye procedures such as these can enhance injury within the eye, resulting in vitreous detachments.
Floaters and Flashes Definition Video
Treatment for Spots and Floaters
Most eye floaters and spots are safe and simply irritating. Lots of will fade with time and become less irritating.
Sometimes people are interested in surgery to remove eye floaters, however physicians agree to carry out such surgery just in rare circumstances when vision seriously is hampered.
At this time, the only way to “clear” the vitreous and its specks and webs would be to eliminate the gel-like substance totally from the eye through a vitrectomy procedure. Generally, the vitreous then is changed with a saline liquid.
Bear in mind that the unexpected appearance of a significant variety of eye floaters, especially if they are accompanied by flashes of light or other vision disruptions, might indicate a removed retina or other major issue in the eye. A retinal detachment or tear is an emergency situation, requiring instant interest.
If you unexpectedly see brand-new floaters, visit your eye doctor without hold-up.