Low hemoglobin level means your blood doesn’t carry enough oxygen, because hemoglobin is the protein inside red blood cells that does that job. It’s like running an engine on less fuel — your body can still move, but every task feels heavier and slower. This imbalance often signals something deeper, leading us to ask why the body isn’t making or keeping enough red cells.
A low hemoglobin level, which can appear as mild anemia or a more serious deficiency, affects millions of people worldwide. According to the World Health Organization, anemia — the broader condition behind most low hemoglobin cases — impacts roughly one in four people, especially women and children. The causes range from iron deficiency and chronic illness to genetic conditions and blood loss.
When someone constantly feels weak, pale, or short of breath — especially after minimal effort — it’s worth understanding what’s happening inside the bloodstream. Looking closely at the mechanisms behind a low hemoglobin level helps explain these symptoms and points to the steps needed to restore balance and health.
What Causes a Low Hemoglobin Level?
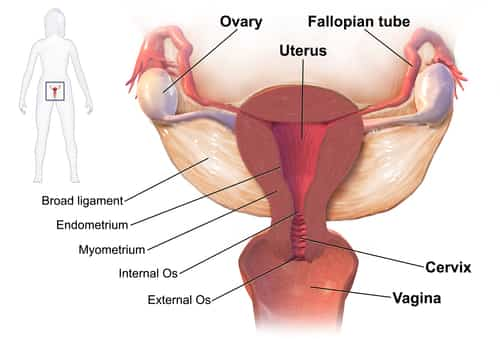
Low hemoglobin (Hb) levels can result from various causes, ranging from nutritional deficiencies to chronic diseases. The most common culprit is iron deficiency, which reduces the body’s ability to produce healthy red blood cells. Other causes include vitamin B12 and folate deficiency, chronic kidney disease, blood loss (menstrual, gastrointestinal, or surgical), and genetic conditions such as sickle cell anemia or thalassemia.
Common Causes and Their Frequency in the U.S.
| Cause | Approximate Prevalence | Notes |
|---|---|---|
| Iron deficiency | 3% of adults | Most common cause of anemia |
| Chronic kidney disease | 1 in 7 adults | Reduced erythropoietin production |
| Vitamin B12 deficiency | 6% of adults over 60 | Poor absorption or diet |
| Folate deficiency | 2% overall | Often due to poor diet |
| Blood loss | Variable | Common in women and post-surgery |
Low hemoglobin causes often overlap; for example, chronic disease can exacerbate nutritional deficiency [source].
What Are the Symptoms of Low Hemoglobin?
Low hemoglobin affects nearly every organ system because oxygen transport is compromised. Recognizing the symptoms early helps prevent progression to severe anemia. Below is a comprehensive list of common symptoms with short explanations of what they typically look like in daily life.
Common Symptoms Explained
- Fatigue and lack of energy: Persistent tiredness even after a good night’s sleep. Often most noticeable in the morning or after mild activity, as tissues don’t receive enough oxygen to sustain energy levels.
- Pale or yellowish skin: Caused by reduced red blood cell count and oxygen delivery. The skin appears lighter than usual, especially on the face, lips, and palms — noticeable year-round, not just in colder months.
- Shortness of breath: Breathing becomes shallow or rapid during routine tasks, such as walking up stairs. This happens because the body compensates for lower oxygen by increasing respiration.
- Dizziness or lightheadedness: Feeling faint or unstable when standing up quickly. Due to reduced oxygen flow to the brain.
- Cold hands and feet: Caused by decreased blood circulation to extremities. Common even in moderate temperatures.
- Chest pain or irregular heartbeat: The heart works harder to pump oxygen-rich blood, which can lead to palpitations or mild chest discomfort, especially during exertion.
- Headaches and concentration problems: The brain’s oxygen shortage may trigger frequent headaches, mental fog, or difficulty focusing at work.
- Brittle nails and hair loss: Long-term oxygen deficiency weakens keratin production, leading to fragile nails or increased hair shedding.
- Unusual cravings (pica): Some individuals develop cravings for non-food items like ice or clay, a telltale sign of iron deficiency anemia.
- Restless legs syndrome: Tingling or uncomfortable sensations in the legs, particularly at night, linked to iron deficiency and disrupted dopamine function.
These symptoms can vary in severity depending on the underlying cause. For instance, people with chronic kidney disease may develop anemia gradually and experience fewer symptoms at first, while those with sudden blood loss often feel abrupt weakness and dizziness.
Real Case (U.S.): Female, 42, from Chicago, experienced persistent exhaustion, pale skin, and shortness of breath during daily chores. Her CBC showed hemoglobin at 9.5 g/dL (95 g/L), leading to a diagnosis of iron-deficiency anemia.
How Is Low Hemoglobin Diagnosed?
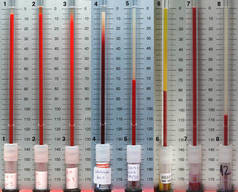
Diagnosis begins with a Complete Blood Count (CBC), the gold standard test for detecting anemia. However, physicians often combine several tests to pinpoint the cause and determine the most effective treatment.
Complete Blood Count (CBC): The Gold Standard
The CBC test is the first and most important step. A small blood sample is drawn from a vein in your arm using a sterile needle. The blood is then analyzed by an automated machine that measures your hemoglobin concentration, hematocrit (percentage of red blood cells in the blood), and red blood cell size and count. The process takes only about 5–10 minutes, and results are typically ready within a few hours to one day, depending on the lab. This test gives a clear overview of whether anemia is present and how severe it is.
Iron Studies and Ferritin Test
If the CBC shows low hemoglobin, the next step is to determine whether iron deficiency is the cause. These tests measure serum iron, ferritin (iron storage protein), total iron-binding capacity (TIBC), and transferrin saturation. Blood is drawn in a similar way, and the sample is analyzed to see how much iron your body has available and stored. The process takes about 10 minutes, and results are usually available within 24–48 hours. High TIBC and low ferritin typically indicate iron deficiency.
Reticulocyte Count
This test measures how quickly new red blood cells (reticulocytes) are being produced in the bone marrow. A small blood sample is taken and examined under a microscope or with an automated counter. It helps doctors understand whether your bone marrow is producing enough new cells. The procedure takes less than 10 minutes, with results available within a day. It’s essential for differentiating between blood loss anemia and bone marrow disorders.
Bone Marrow Biopsy
This is a more advanced diagnostic method used when the cause of low hemoglobin remains unclear. A doctor numbs a small area (usually the hip bone) and removes a tiny sample of bone marrow using a special needle. The sample is examined under a microscope to assess red and white cell production. The procedure takes about 30 minutes, and recovery is quick — mild soreness for a day or two. Results are ready within 3–5 days. It’s a highly accurate way to detect blood cancers or bone marrow failure.
Genetic Tests
If hereditary anemia (like sickle cell or thalassemia) is suspected, doctors may order genetic tests. A simple blood or saliva sample is collected, and DNA is analyzed in a laboratory to identify gene mutations affecting hemoglobin production. The test takes about 15 minutes to collect the sample, and results are typically available within 1–2 weeks. These tests provide valuable insight for families with a history of inherited blood disorders.
Diagnostic Tests, Accuracy, and Average Cost
| Test | Accuracy (1–10) | Average Cost (USD) |
|---|---|---|
| CBC | 9 | 30–50 |
| Ferritin | 8 | 50–120 |
| Reticulocyte count | 9 | 80–150 |
| Bone marrow biopsy | 10 | 500–1500 |
| Genetic test | 10 | 300–1000 |
How Do Doctors Treat Low Hemoglobin Today?
Treatment for low hemoglobin depends on its cause, severity, and how quickly the levels need to be restored. The goal is simple: increase oxygen-carrying capacity and fix the root cause. Here’s what each treatment involves and what patients can expect.
Iron Supplements and IV Therapy
Iron therapy is the backbone of anemia treatment. When your body lacks iron, it cannot make enough red blood cells — think of it as trying to bake bread without flour. Oral iron supplements such as Ferrex 150, Slow Fe, and Feosol are typically the first step. They come in tablets or liquid form and are taken daily for 2 to 6 months, depending on the severity. Improvements are usually seen within 2–3 weeks, but full recovery takes longer as the body replenishes its iron stores. Side effects can include mild constipation or stomach upset, which can be reduced by taking iron with food (though it slightly lowers absorption).
For patients who cannot tolerate oral iron or need faster correction, intravenous (IV) iron therapy is an alternative. Brands like Venofer and Injectafer deliver iron directly into the bloodstream in a controlled environment — typically an outpatient clinic or hospital infusion center. Each session lasts 30–60 minutes, and 2–4 sessions may be required. The results are often noticeable within a week, especially for those with severe anemia or chronic kidney disease. The average cost is around $400–800 per infusion, depending on location and insurance coverage.
Vitamin and Folate Therapy
Low hemoglobin may also result from vitamin B12 or folate (vitamin B9) deficiency. These nutrients are essential for red blood cell production in the bone marrow. Treatment usually involves B12 injections (Cyanocobalamin) once a week for a month, then monthly for maintenance. Patients who dislike injections can use sublingual B12 tablets like Nature’s Bounty B12. Folate deficiency is corrected with oral supplements like Folvite (1–5 mg daily). Most people begin to feel better within 2–4 weeks, as their red blood cell counts gradually rise. Average monthly cost ranges from $20–$50.
Erythropoiesis-Stimulating Agents (ESAs)
In chronic diseases such as kidney failure or chemotherapy-induced anemia, the body stops producing erythropoietin — the hormone that signals the bone marrow to make red cells. ESAs like Epogen and Aranesp replace this hormone. The treatment is given as a small injection under the skin or into a vein, typically once every 1–4 weeks. It’s often combined with iron therapy for best results. Patients usually notice improvement in fatigue and exercise tolerance within 2–3 weeks. ESAs are expensive, costing over $1000 per dose, but they are life-changing for patients with chronic illness.
Blood Transfusions
For dangerously low hemoglobin levels (below 7 g/dL or 70 g/L), a blood transfusion is often necessary. The process involves receiving compatible donor red blood cells through an IV line. It usually takes 2–4 hours, and patients can feel improvement in energy and breathing within hours after the procedure. Blood transfusions are carefully matched and monitored to prevent reactions. While they are effective immediately, they are considered temporary support — a “boost,” not a fix. The average cost ranges from $1,000 to $3,000 per unit of blood.
Emerging Technologies
Medicine is advancing toward alternatives to transfusion. Research companies such as Oxygen Therapeutics, Inc. are developing artificial oxygen carriers (AOCs) — lab-made molecules that can transport oxygen like natural hemoglobin. Though still in clinical trials, these could revolutionize emergency care and reduce dependence on blood donors. Hospitals in the U.S. are also experimenting with high-efficiency erythropoiesis analyzers that personalize iron and ESA dosages, improving results and reducing side effects.
Can Diet Really Help Boost Hemoglobin?
Absolutely. Diet plays a major role in maintaining hemoglobin levels. Iron-rich foods like red meat, liver, spinach, lentils, and quinoa are excellent sources. Pairing iron with vitamin C (like citrus fruits) boosts absorption significantly.
Top Foods to Increase Hemoglobin (per 100 g)
| Food | Iron (mg) | Notes |
|---|---|---|
| Beef liver | 6.2 | High in heme iron |
| Spinach | 2.7 | Best absorbed with vitamin C |
| Lentils | 3.3 | Great plant-based source |
| Quinoa | 1.5 | Gluten-free grain option |
| Chicken | 1.3 | Moderate heme iron source |
Reyus Mammadli, medical consultant, recommends consuming iron with vitamin C and avoiding tea or coffee with meals to improve absorption.
When Should You See a Doctor for Low Hemoglobin?
You should consult a healthcare provider if you notice persistent fatigue, pale skin, or unexplained weakness. Seek immediate attention if you experience shortness of breath, chest pain, or irregular heartbeat.
Reyus Mammadli advises: “Don’t ignore the signs — anemia can sneak up like a quiet roommate.” Regular blood testing is crucial, especially for women and older adults.
Prevention and Lifestyle Tips
Maintaining balanced nutrition, addressing chronic illnesses, and avoiding unnecessary blood loss are key preventive strategies. Regular exercise improves oxygen utilization, while a diet rich in iron, folate, and B12 supports red blood cell production.
Quick Tips:
- Include lean meat and leafy greens daily
- Combine iron and vitamin C sources
- Avoid excessive caffeine during meals
- Schedule CBC checks yearly
Editorial Advice
According to medical consultant Reyus Mammadli, the best approach to low hemoglobin is early detection and a combination of nutrition and targeted therapy. Modern diagnostic tools such as automated CBC analyzers and genetic screening allow physicians to identify underlying causes faster and treat more precisely.
Editorial Team Advice: Keep track of your blood test results, eat smart, and don’t self-medicate with iron supplements without medical supervision. Hemoglobin health is all about balance — both in your body and lifestyle.





thankyou for this information, I have chronic kidney disease and my blood tests always showed low hemoglobin, and anemia I am just starting today fefol iron and folic acid capsules, lets hope this helps, and is safe to take if you have kidney disease. I do feel more confident now I have read the information you provided.