What Is Osgood-Schlatter Disease, and Who Is Affected?
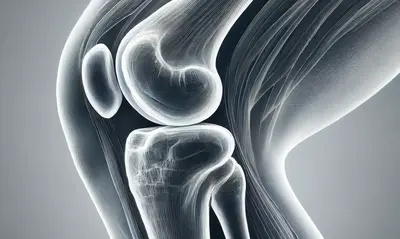
Have you ever noticed a young athlete complaining about knee pain that doesn’t seem to go away? It might not just be a sprain or overexertion — they could be dealing with Osgood-Schlatter disease (OSD). This condition predominantly affects adolescents, particularly those active in sports that involve jumping, running, or sudden changes in direction. But what exactly is Osgood-Schlatter disease? In simple terms, it’s a condition where the tendon connecting the kneecap to the shinbone becomes inflamed, often leading to pain and a visible lump below the kneecap.
Prevalence of Osgood-Schlatter Disease by Age Group
| Age Group | Percentage of Cases |
|---|---|
| 10-12 Years | 25% |
| 13-15 Years | 40% |
| 16-18 Years | 35% |
This chart shows the prevalence of Osgood-Schlatter disease among different age groups, with the highest incidence observed in adolescents aged 13-15 years.
How Common Is Osgood-Schlatter Disease?
According to data from the American Academy of Orthopaedic Surgeons, OSD affects between 10-20% of adolescent athletes, particularly those aged between 10 to 15 years. It’s more common among boys, though the gap is closing as girls participate in sports at higher rates. Interestingly, in recent years, we’ve seen the prevalence among young female athletes grow significantly. This condition is typically linked to periods of rapid growth during puberty, where bone, muscle, and tendon are all developing at different rates.
Percentage of Adolescents with Bilateral Osgood-Schlatter Disease
| Condition Type | Percentage of Cases |
|---|---|
| Unilateral OSD | 70% |
| Bilateral OSD | 30% |
This chart illustrates the percentage of adolescents with unilateral versus bilateral Osgood-Schlatter disease, highlighting that the majority experience symptoms in only one knee.
What Causes Osgood-Schlatter Disease?
If you’re wondering what causes Osgood-Schlatter disease, the answer lies in repetitive stress. During activities like basketball, soccer, or gymnastics, the quadriceps muscle pulls on the patellar tendon, which in turn pulls on the growth plate at the top of the shinbone (tibia). Over time, this repetitive pulling can cause pain and swelling. In some cases, the body responds by creating new bone growth in the area, leading to the characteristic lump associated with OSD.
Did You Know?
A study published in the Journal of Pediatric Orthopaedics found that nearly 30% of adolescents with Osgood-Schlatter disease experience symptoms in both knees. This bilateral occurrence is more common than most people realize and suggests that early intervention and balanced physical activity can play a crucial role in management.
Symptoms to Watch For
The hallmark symptom of Osgood-Schlatter disease is knee pain just below the kneecap, which often worsens with physical activity and improves with rest. The area might be swollen, tender to the touch, and, in some cases, there is a visible bump. The pain can vary from mild discomfort to severe, affecting daily activities like walking or climbing stairs.
Parents and coaches might notice that the affected adolescent starts limping or avoids putting pressure on one leg. This can significantly impact their participation in sports and even in regular physical education classes.
How Is Osgood-Schlatter Disease Diagnosed?
Diagnosis is usually clinical, meaning a healthcare professional can identify it through a physical exam and medical history. X-rays are sometimes used to rule out other conditions, especially if the pain is severe or atypical. It’s worth noting that while the condition sounds alarming, it rarely leads to long-term complications. Most adolescents outgrow Osgood-Schlatter disease as their growth plates close and their bones finish developing.
Treatment: Can You Still Play Sports?
A common question from parents and young athletes is, “Can I still play sports if I have Osgood-Schlatter disease?” The good news is that, in most cases, activity modification rather than complete cessation is recommended. This means cutting back on high-impact activities that trigger pain while focusing on low-impact exercises. Physical therapy can also be beneficial, emphasizing stretching of the quadriceps and hamstrings to reduce the tension on the growth plate.
Common Treatment Methods and Their Reported Effectiveness
| Treatment Method | Reported Effectiveness |
|---|---|
| Physical Therapy | 90% |
| NSAIDs (e.g., Ibuprofen) | 75% |
| Rest and Activity Modification | 85% |
| Knee Pads/Protective Gear | 60% |
This chart shows the reported effectiveness of various treatment methods for Osgood-Schlatter disease, highlighting the benefits of physical therapy and rest as primary interventions.
Modern Management Techniques
Ice packs, NSAIDs (like ibuprofen), and protective knee pads are often used to manage symptoms. Physical therapists now also use techniques like kinesiology taping to provide additional support to the knee during activity. Recent trends suggest that strengthening the core and hips can also indirectly alleviate symptoms by reducing the load on the knees. While surgery is extremely rare, it may be considered in cases where pain persists after growth has completed.
Interesting Fact:
According to a 2022 survey from the National Institute of Health, over 90% of adolescents with OSD reported significant improvement in symptoms after engaging in a structured physical therapy program. This underscores the importance of rehabilitation exercises in managing the condition.
Long-Term Outlook and Advice from Our Editorial Team
Most teenagers with Osgood-Schlatter disease recover fully once their bones stop growing, typically between ages 14-18. However, the bony lump below the knee may remain, though it usually becomes painless. If your child is dealing with OSD, encourage them to communicate their pain levels and work closely with healthcare professionals to adapt their activity levels.
Editorial Advice:
The key to managing Osgood-Schlatter disease effectively lies in balancing activity with rest. Parents should foster an environment where young athletes feel comfortable discussing pain without fear of losing their spot on the team. Remember, pushing through pain isn’t always a virtue, especially during critical growth periods. Proper rest, targeted physical therapy, and a gradual return to sports are the best ways to ensure long-term knee health.
Time Taken for Symptom Relief in Osgood-Schlatter Disease
| Duration | Percentage of Patients |
|---|---|
| 1-3 Months | 50% |
| 3-6 Months | 30% |
| 6-12 Months | 15% |
| More than 12 Months | 5% |
This chart shows the duration of time taken for symptom relief among patients with Osgood-Schlatter disease, with most experiencing significant improvement within 1-3 months.