Radiotherapy, also called radiation therapy, is the treatment of cancer and other illness with ionizing radiation. Ionizing radiation deposits energy that hurts or damages cells in the area being dealt with (the target tissue) by damaging the genetic product (DNA) in the individual cells, making it difficult for them to continue to grow.
Although radiation damages both cancer cells and regular cells, normal, healthy cells are able to fix themselves and return to proper functioning. Radiotherapy may be utilized to treat localized solid tumors, such as those cancers related to the oral environment. It can likewise be utilized to deal with leukemia and lymphoma (cancers of the blood-forming cells and lymphatic system, respectively).
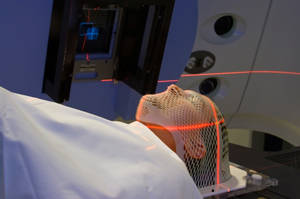
Prior to starting radiation therapy treatments a planning session, or simulation, is performed. This involves special x-rays or CAT scan images and measurements of the area to be treated, as well as markings (long lasting, but not long-term tattoos) being placed on the patient’s skin to assist with positioning during the real treatments. This planning session might take up to an hour to finish, however is vital in providing information for ideal treatment planning. For oral cancers, along with a lot of head and neck cancers, a permeable mesh mask will be made during this treatment. When used in the radiation treatment space, the mask paralyzes the patients’ head throughout treatment. This is crucial so that radiation will only be provided to the designated areas.
The total dosage of radiation treatment recommended by the radiation oncologist is broken down into percentages (portions) which are offered on an everyday basis, usually five days in a row with a two day break each week. It has actually been discovered that patients much better tolerate the smaller sized everyday doses while still receiving the maximum benefit of the treatments. Usually, each day-to-day treatment lasts about 10 to 15 minutes, with the majority of this time spent making certain the radiation obstructing devices, which limit the radiation to the proper area are correctly in location, and the patient and device are properly placed. It really takes more time to establish the machine and the patient than it does to provide the dose of radiation. The employee who are accountable for managing the daily radiation therapy treatments have gotten specialized education and accreditation and are called radiation therapists.
The reason that the treatment course for some cancers is so reasonably long (2-8 weeks) is to permit typical tissue repair after each exposure to radiation, and to minimize permanent injury. (Tissue repair can also be assisted by appropriate nutrition and a positive frame of mind. See suggestions for nutrition during treatment in other places on this website.) The everyday dose has to also be great enough to destroy the cancer cell while sparing the regular tissues of excessive levels of radiation. This balancing act forms the basis of modern radiation therapy
Types of Radiation Therapy for Tongue Cancer
One type of radiation treatment frequently made use of includes photons, “packets” of energy. X-rays were the first kind of photon radiation to be made use of to treat cancer. Depending on the quantity of energy they possess, the rays can be utilized to destroy cancer cells on the surface area of an area, or permeate to tissues deeper in the body. The greater the energy of the x-ray beam, the deeper the x-rays can go into the target tissue. Linear accelerators and betatrons are machines that produce x-rays of increasingly greater energy. The use of machines to focus radiation (such as x-rays) on a cancer website is called external beam radiotherapy. With modern radiation devices, there is very little scatter of x-ray energy outside the treatment beam. Scatter refers to the existence of radiation in the body outside the field of treatment. Imagine a beam from a flashlight predicted on a wall. The visible beam of the light is well specified (comparable to the radiation beam) with only a small halo of light around the edges (comparable to the scatter). In radiation treatment, a greatly defined x-ray beam lessens the side effects of treatment since only small amounts of radiation travel to other parts of the body.
Gamma rays are another form of photons used in radiotherapy. Gamma rays are produced spontaneously as specific aspects (such as radium, uranium, and cobalt 60) release radiation as they decay, or degeneration. Each component decomposes at a certain rate and emits energy through gamma rays and other particles. X-rays and gamma rays have the very same result on cancer cells.
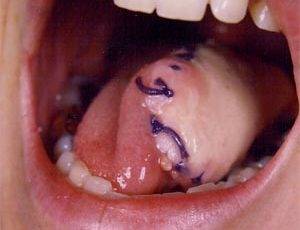
Another technique for providing radiation to cancer cells is to put radioactive implants straight into a tumor or body cavity. This is called internal radiotherapy. (Brachytherapy, interstitial irradiation, and intracavitary irradiation are kinds of internal radiotherapy.) In this treatment, the radiation dose is focused in a little area. Internal radiotherapy is often utilized for cancers of the tongue, uterus, prostate, and cervix. One of the benefits of this kind of treatment is there is less radiation exposure to other parts of the body.
Numerous new methods to radiation therapy are being examined to determine their effectiveness in dealing with tongue cancer. One such strategy is intraoperative irradiation, in which a big dosage of external radiation is directed at the growth and surrounding tissue throughout surgery. Another investigational strategy is particle beam radiation therapy. This type of treatment varies from photon radiotherapy in that it includes using fast-moving subatomic particles to deal with localized cancers. A really advanced device is had to produce and speed up the particles needed for this procedure. Some particles (neutrons, pions, and heavy ions) deposit more energy along the course they take through tissue than do x-rays or gamma rays, hence causing more damage to the cells they hit. This type of radiation is frequently referred to as high linear energy transfer (high LET) radiation.
Scientists also are looking for ways to enhance the efficiency of existing radiation therapy methods. 2 types of investigational drugs are being studied for their effect on cells undergoing radiation. These drugs called Radiosensitizers, make the growth cells more likely to be damaged, and other drugs called radioprotectors, safeguard regular tissues from the effects of radiation. Hyperthermia, or using heat, is likewise being studied for its efficiency in sensitizing tissues to radiation.
Other recent radiotherapy research study has actually focused on the use of radiolabeled antibodies to deliver doses of radiation directly to the cancer website (radioimmunotherapy). Antibodies are extremely certain proteins that are made by the body in reaction to the presence of antigens (substances recognized as foreign by the body immune system). Some tumor cells contain certain antigens that set off the body’s immune system to produce tumor-specific antibodies. Huge quantities of these antibodies can be made in the laboratory and attached to radioactive compounds (a process known as radiolabeling). Once injected into the body, the antibodies actively seek the cancer cells, which are destroyed by the cell-killing (cytotoxic) action of the radiation. The benefit to this technique is that it can decrease the danger of radiation damage to the body’s healthy cells. The success of this strategy will depend upon both the recognition of appropriate radioactive compounds and decision of the safe and reliable dosage of radiation that can be provided in this way.
Radiotherapy therapy for tongue cancer might be used alone or in combination with chemotherapy or surgery. Like all types of cancer treatment, radiation treatment can have side effects. Possible side effects of treatment with radiation include temporary or long-term loss of hair in the area being treated, moderate to severe skin inflammation, temporary modification in skin color in the cured area, nausea, and fatigue. Direct exposure of the mouth to radiation will produce mucositis, making the interior of the mouth quite sore. This will solve after the radiation treatments have been finished. Another complication associated with radiation treatment of the oral cavity or throat, is xerostomia. It is not unusual to have the salivary glands harmed during the course of treatment. This leads to an irreversible loss of salivary function (xerostomia). New techniques such as IMRT (strength regulated radiotherapy) are being implemented at more cancer centers, which can avoid this civilian casualties to the salivary glands. Making use of a different software program to provide the radiation from numerous angles in smaller sized dosages, this method likewise includes a new shuttering device to restrict the size of the radiation beams which are emitted, thus missing out on the glands and sparing them any direct exposure to the harmful radiation.