Adults with cancer may be at risk for constraints in functional status and quality of life (QOL). Occupational therapy is a supportive service with the specific mission to help people functionally engage in life as safely and independently as possible with the primary goal of improving QOL. Sadly, for people with cancer, occupational therapy stays underused. The overall purpose of this review is to provide an understanding of what occupational therapy is and its importance to patients with cancer, highlight the needs to refer, and, last, offer basic advice on how to access services.
Occupational Therapy
Occupational therapy uses a variety of techniques and tools to improve functional capacity. Goals are written in cooperation with the patient to identify the activities essential to their quality of life (QOL). Occupational therapy can increase practical status, reduce risk of falling, improve social involvement, and improve general QOL. Occupational therapy interventions also improve life fulfillment and participation in one’s life roles, pain control, and total psychological health. Occupational therapy interventions can result in improvements simply put- and long-term results and are cost effective.
Falls
Older adults with cancer are at a higher risk for falls compared with those without cancer. In one study, 44% of the patients who fell also reported a restriction in IADLs. Yet, studies have actually regularly reported that oncology providers hardly ever report a fall or respond with appropriate and prompt intervention. For fall prevention in community-dwelling older adults, the most reliable interventions consist of home adjustments and adaptations, which are most reliable when finished by a physical therapist. In a randomized control trial of older adults, home occupational therapy decreased the risk of falling in those who had fallen in the past.
Cognitive Function Impairment
Cancer-related cognitive problems (CRCI) provides as troubles related to memory, attention, information-processing speed, and organization, and can impact all age groups. For example, women with breast CRCI report mild cognitive decrease affecting their ability to function, making formerly easy activities more difficult and causing stressful loss of self-reliance in family life functions. For this problem, occupational therapy intervention will pursue adapting or remediating the practical disability through different cognitive techniques. The physical therapist will normally incorporate adaptive techniques so that the patient discovers how to compensate for impaired memory or attention while carrying out particular jobs, or use restorative activities to enhance cognition functions during the efficiency of particular jobs.
Cancer-Related Fatigue
Cancer-related fatigue (CRF) is a commonly reported issue amongst cancer survivors that can interrupt day-to-day routines and restrict involvement in meaningful activity. Ninety-one percent of adults with cancer report tiredness as a symptom that has “avoided them from leading a ‘normal’ life” and 88% need to modify their daily routine. Patients with CRF can take advantage of energy preservation training taught in occupational therapy. This equates into useful strategies to manage tiredness for resumption of functions and regimens. Structured activity modification and prioritization, along with use of an everyday activity log to keep track of task-based activity and energy patterns, belong of this training. Patients therefore have actually individualized modifications (e.g., putting frequently used items in the fridge at easy-to-reach heights, timing showers in the evening) to conserve energy to take pleasure in the activities that contribute most to their QOL.
Upper-Extremity Impairments
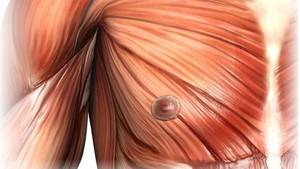
In breast and other cancers, surgery has the potential to cause short- and long-lasting physical disabilities that are potentially flexible with occupational therapy. Limited upper-extremity series of movement, arm swelling (lymphedema), pain, and numbness are all common disabilities of the upper extremity in patients after surgery for breast cancer. Special needs related to arm variety of motion was usually connected with ADL and IADL disabilities such as putting on a sweater, making a bed, doing backyard work, bring groceries, and raising anything weighing more than 10 pounds (i.e., children).
Occupational therapy for patients with restrictions in their upper extremities could include a combination of workout, extending, and modalities to enhance variety of motion and muscle strength, followed by training in the performance of functional tasks and adjustment of the activity or environment, as required. Numerous tools commonly used and suggested by occupational therapists can enhance self-reliance (e.g., a rocker knife used to cut food using one hand) and limit the result of upper-extremity limitations on QOL.
Lymphedema
Lymphedema causes reduced QOL, modified body image, decreased work/leisure involvement, and impaired occupational engagement. Occupational therapists can assist patients determine significant activities and use activity adjustments for effective conclusion, use stress management and relaxation techniques to decrease anxiety, and address issues associated with modifications in body image. Lymphedema education consists of the identification of risk for worsening and activities that might worsen the swelling, appropriate activity adjustments, energy conservation strategies, self-massage, and management of the swelling with total decongestive therapy.
Chemotherapy-Induced Peripheral Neuropathy
Paclitaxel, docetaxel, vincristine, oxaliplatin, cisplatin, and taxanes can possibly cause chemotherapy-related peripheral neuropathy [39] Patients might experience weak point, numbness, tingling, and/or pain in their extremities that can lead to lowered QOL. Patients with chemotherapy-induced sensory neuropathy report high levels of practical special needs. Adults report difficulty with house cleaning, distinguishing items in their hands (tactile agnosia), and a boost in general dependence on others. Occupational therapy interventions for peripheral neuropathy concentrate on adjustment and remediation through sensory and functional activities (e.g., cooking) and adapting particular tools to keep independence with ADLs and IADLs (e.g., a button hook to assist with attaching buttons when dressing).
Practical Impairments
For adults with cancer, occupational therapists likewise attend to how cancer-specific problems, such as tiredness, cognition, pain, and peripheral neuropathy, may affect changes in practical status and daily routines. For adults who provide with practical impairments, occupational therapy interventions would help with skills ranging from dressing, bathing, and using the toilet, to the more complicated IADL jobs of arranging one’s schedule for the day, balancing a checkbook, cooking, and being able to care for children or aging relatives.