Hormone therapy is another form of systemic therapy. It is frequently utilized as an adjuvant therapy to help decrease the risk of the cancer returning after surgery, but it can be used as neoadjuvant treatment, as well. It is also used to treat cancer that has come back after treatment or has spread.
Breast cancer hormone therapy – how does it work?
A female’s ovaries are the primary source of the hormonal agent estrogen up until menopause. After menopause, smaller sized amounts are still made in the body’s fat tissue, where a hormone made by the adrenal gland is transformed into estrogen.
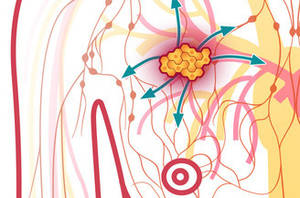
Estrogen promotes the growth of cancers that are hormonal agent receptor-positive. About 2 from 3 of breast cancers are hormone receptor-positive– they consist of receptors for the hormones estrogen (ER-positive cancers) and/or progesterone (PR-positive cancers). Many types of hormone therapy for breast cancer either lower estrogen levels or stop estrogen from acting upon breast cancer cells. This kind of treatment is valuable for hormone receptor-positive breast cancers, however it does not assist patients whose tumors are hormonal agent receptor negative (both ER- and PR-negative).
Breast cancer hormone therapy medications
Tamoxifen: Tamoxifen obstructs estrogen receptors in breast cancer cells. This stops estrogen from binding to them and informing the cells to grow and divide. While tamoxifen acts like an anti-estrogen in breast cells, it acts like an estrogen in other tissues, like the uterus and the bones. Due to the fact that it acts like estrogen in some tissues but like an anti-estrogen in others, it is called a careful estrogen receptor modulator or SERM.
For women with hormonal agent receptor-positive invasive breast cancer, tamoxifen can be provided for 5 to 10 years after surgery to lower the chances of the cancer coming back and helping patients live longer. It also decreases the risk of a brand-new breast cancer in the other breast. For early stage breast cancer, this drug is generally used for women who have not yet gone through menopause. Aromatase inhibitors (talked about listed below) are the favored treatment for women who have actually gone through menopause.
For women who have been dealt with for ductal carcinoma in situ (DCIS) that is hormone receptor-positive, taking tamoxifen for 5 years reduces the chance of the DCIS coming back. It also lowers the opportunity of getting an invasive breast cancer.
Tamoxifen can likewise stop the growth as well as diminish tumors in women with metastatic breast cancer. It can also be made use of to lower the risk of developing breast cancer in women at high risk.
This drug is taken by mouth, frequently as a tablet.
The most typical side effects of these drugs include tiredness, hot flashes, vaginal dryness or discharge, and state of mind swings.
Some women with bone metastases may have a “tumor flare” with pain and swelling in the muscles and bones. This generally subsides rapidly, however in some uncommon cases a woman may likewise develop a high calcium level in the blood that can not be managed. If this takes place, the treatment might need to be picked up a time.
Unusual, but more severe side effects are likewise possible. These drugs can enhance the risk of developing cancers of the uterus (endometrial cancer and uterine sarcoma) in women who have actually gone through menopause. Inform your doctor right away about any unusual vaginal bleeding (a common symptom of both of these cancers). Many uterine bleeding is not from cancer, but this symptom constantly needs timely interest.
Blood clots are another possible major side effect. They typically form in the legs (called deep venous apoplexy or DVT), but in some cases a piece of clot may break off and wind up blocking an artery in the lungs (lung embolism or PE). Call your doctor or nurse right away if you develop pain, soreness, or swelling in your lower leg (calf), shortness of breath, or chest pain due to the fact that these can be symptoms of a DVT or PE.
Rarely, tamoxifen has actually been connected with strokes in post-menopausal women so tell your doctor if you have severe headaches, confusion, or problem speaking or moving.
These drugs may likewise increase the risk of a heart attack.
Depending on a lady’s menopausal status, tamoxifen can have different effects on the bones. In pre-menopausal women, tamoxifen can cause some bone thinning, but in post-menopausal women it is frequently good for bone stamina.
The advantages of taking these drugs exceed the risks for nearly all women with hormone receptor-positive invasive breast cancer.
Toremifene (Fareston ®): Toremifene is a drug much like tamoxifen. It is likewise a SERM and has similar side effects. It is just authorized to treat metastatic breast cancer. This drug is not likely to work if tamoxifen has been made use of and quit working.
Fulvestrant (Faslodex ®): Fulvestrant is a drug that first obstructs the estrogen receptor and then also removes it temporarily. It is not a SERM– it acts like an anti-estrogen throughout the body.
Fulvestrant is utilized to treat advanced (metastatic breast cancer), frequently after other hormonal agent drugs (like tamoxifen and frequently an aromatase inhibitor) have quit working.
It is provided by injections into the butts. For the first month, the shots are given 2 weeks apart. After that, it is offered as soon as a month. Common short-term side effects can consist of hot flashes, night sweats, moderate queasiness, and fatigue. Because it obstructs estrogen, in theory it could weaken bones (osteoporosis) if it is taken for a long period of time.
It is currently just approved by the FDA for use in post-menopausal women with sophisticated breast cancer that not reacts to tamoxifen or toremifene. It is sometimes made use of “off-label” in pre-menopausal women, frequently combined with a luteinizing-hormone launching hormonal agent (LHRH) agonist to turn off the ovaries (see below).
Treatments to lower estrogen levels
Aromatase inhibitors (AIs): Three drugs that stop estrogen production in post-menopausal women have been approved to deal with both early and advanced breast cancer: letrozole (Femara), anastrozole (Arimidex), and exemestane (Aromasin). They work by blocking an enzyme (aromatase) in fat tissue that is accountable for making small quantities of estrogen in post-menopausal women. They can not stop the ovaries from making estrogen, so they are just efficient in women whose ovaries aren’t working, either due to menopause or due to treatment with luteinizing hormone-releasing hormone analogs (these are gone over in the future). AIs are taken daily as pills. Up until now, drugs in this group seem to work equally well in dealing with breast cancer.
A number of researches have compared these drugs to tamoxifen as adjuvant (after surgery) hormonal agent therapy in post-menopausal women. Utilizing these drugs, either alone or after tamoxifen, has been revealed to better decrease the risk of the cancer coming back later than utilizing simply tamoxifen for 5 years. Schedules that are known to be practical include:
- Tamoxifen for 2 to 3 years, followed by an aromatase inhibitor (AI) to finish 5 years of treatment
- Tamoxifen for 5 years, followed by an AI for 5 years
- An AI for 5 years
A lot of doctors now advise post-menopausal women whose cancers are hormone receptor– favorable use an AI eventually during adjuvant hormone therapy for breast cancer. Today, conventional treatment is to make use of these drugs for about 5 years (or alternate with tamoxifen for an overall of at least 5 years). Studies now being done to see if giving an AI for more than 5 years would be more valuable.
For women with early-stage breast cancer who have not gone through menopause when they are first diagnosed, tamoxifen is often utilized first, and after that an AI might be provided later if they go through menopause during treatment. Another option is taking a drug that shuts off the ovaries (a luteinizing hormone-releasing hormonal agent analog) along with an AI.
The AIs tend to have fewer major side effects than tamoxifen– they do not cause uterine cancers and very hardly ever cause embolism. They can, however, cause muscle pain and joint tightness and/or pain. The joint pain may resemble a new sensation of having arthritis in several joints at one time. This side effect might improve by changing to a various AI, however it has led some women to stop drug treatment. If this happens, the majority of physicians advise making use of tamoxifen to complete 5 years of hormonal agent treatment.
Because aromatase inhibitors get rid of all estrogens from women after menopause, they likewise cause bone thinning, sometimes causing osteoporosis as well as fractures. Lots of women treated with an aromatase inhibitor are likewise treated with medication to enhance their bones, such as bisphosphonates or denosumab.
Ovarian ablation: In pre-menopausal women, eliminating or shutting down the ovaries (ovarian oblation), the main source of estrogens, efficiently makes the lady post-menopausal. This may allow some other hormone therapies to work much better and is most often made use of to deal with metastatic breast cancer, but has actually likewise been studied in patients with early-stage disease.
Permanent ovarian ablation can be done by surgically getting rid of the ovaries. This operation is called an oophorectomy. Regularly, ovarian ablation is done with drugs called luteinizing hormone-releasing hormone (LHRH) analogs, such as goserelin (Zoladex ® )or leuprolide (Lupron ®). These drugs stop the signal that the body sends out to ovaries making estrogens. They can be used alone or with other hormone drugs (tamoxifen, aromatase inhibitors, fulvestrant) as hormonal agent therapy in pre-menopausal women.
Chemotherapy drugs may likewise harm the ovaries of pre-menopausal women so they not produce estrogen. In some women, ovarian function returns months or years later, however in others, the damage to the ovaries is irreversible and results in menopause. This can sometimes be a helpful (if unintentional) repercussion of chemotherapy with regard to breast cancer treatment, although it leaves the lady sterile.
All of these techniques can cause a female to have symptoms of menopause, including hot flashes, night sweats, vaginal dryness, and state of mind swings.
Less commonly used types of hormone therapy for breast cancer
These choices were used regularly in the past, but are hardly ever offered now. Megestrol acetate (Megace ®) is a progesterone-like drug used that can be utilized as a hormonal agent treatment of sophisticated breast cancer, usually for women whose cancers do not react to the other hormone treatments. Its significant side effect is weight gain, and it is sometimes made use of in higher doses to reverse effective weight loss for individuals with innovative cancer.
Androgens (male hormones) may seldom be considered after other hormone treatments for advanced breast cancer have been tried. They are in some cases efficient, however they can cause manly characteristics to develop such as a boost in body hair and a much deeper voice.
Another choice that may hardly ever be attempted when the cancer is no longer responding to other hormone drugs is giving high dosages of estrogen. The main risk is of major blood clots (like DVTs and PEs). This treatment can likewise cause nausea.
Breast Cancer: Survival Rate
The outlook for breast cancer differs according to whether the cancer is identified early or when it is advanced. The earlier a breast cancer is diagnosed, the smaller sized it is likely to be and the lower the possibility that it has spread out. The outlook will likewise depend on different other factors, consisting of the grade of the cancer and whether the cells have receptors for specific hormonal agents or biological therapies.
Survival data are readily available for each stage of breast cancer in one area of England. These figures are for women diagnosed between 2002 and 2006.
For stage 1 breast cancers around all women (99 %) will make it through for 5 years or more after medical diagnosis.
For stage 2 breast cancers practically 90 out of 100 women (90 %) will make it through for 5 years or more after medical diagnosis.
Practically 60 from 100 women with stage 3 tumours (60 %) will make it through for 5 years or more after diagnosis.
In 5 in 100 women (5 %), the cancer has actually already infected another part of their body when they are first identified. Regretfully, the outlook as soon as a cancer has infected another body organ is not so excellent. It is not treatable at this moment, but might be managed with treatment for some years. 15 from 100 women with stage 4 tumours (15 %) will make it through for 5 years or more after they are identified.