Runners often finish a great session only to feel a stab or deep ache in one heel minutes later. Whether it’s the right or left side, post‑run heel pain can turn training plans upside down. The good news: most cases respond to smart self‑care and targeted treatment—no heroic measures required.
Common Causes of Post‑Run Heel Pain (Runners)
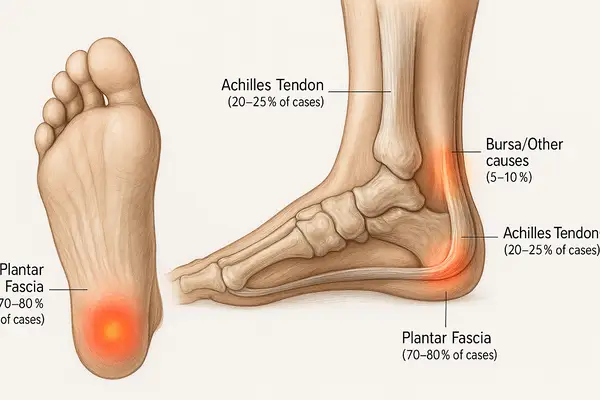
Share of cases in a typical sports‑medicine cohort (percent of heel‑pain presentations).
Plantar fasciopathy 70%
Achilles tendinopathy 20%
Retrocalcaneal bursitis 7%
Calcaneal stress fractures 3%
Bars use a minimum visual width to preserve readability on small screens; numeric labels show the exact values.
Source: iytmed.com
Side‑specific pain (right vs left) usually points to how a runner moves: slight gait asymmetry, habitual cambered roads, or a shoe mismatch can load one heel more than the other. That’s not a character flaw—just biomechanics doing biomechanics.
Clinically, plantar fasciitis (more precisely, plantar fasciopathy) is the leading cause of adult heel pain, with a lifetime incidence around 10% in population studies. Recreational and competitive runners sit squarely in the risk group ⧉.
What are the most likely causes of post‑run heel pain?
Short answer: plantar fasciopathy tops the list, but several other culprits can masquerade as the same ache. Here’s the lay of the land—no fluff, just the greatest hits.
- Plantar fasciopathy (plantar fasciitis): Classically a sharp, first‑step pain in the morning or after sitting, then easing with movement. Pain sits near the medial calcaneal tubercle. Risk rises with rapid mileage jumps, standing on hard floors, decreased ankle dorsiflexion, and certain foot morphologies. The 2023 heel pain clinical practice guideline (JOSPT) remains the North Star for evidence‑based care.
- Insertional or mid‑portion Achilles tendinopathy: Posterior heel pain that worsens with hills or speedwork; palpable thickening or tenderness along the tendon. Calf stiffness is common.
- Retrocalcaneal bursitis/Haglund’s impingement: Pain and swelling just above the posterior heel where a firm heel counter rubs. Often aggravated by narrow, rigid heel cups.
- Calcaneal stress reaction or stress fracture: Deep, focal pain with impact that lingers at rest. Hop tests hurt; squeezing the heel may reproduce pain.
- Medial/lateral plantar nerve entrapment or Baxter’s neuritis: Burning or tingling at the heel/arch border; may worsen in tight footwear.
Heads‑up: runners frequently have more than one issue at once (for example, plantar fascia irritation plus calf tightness). That’s why a thorough exam is the real MVP.
Why does the right heel vs the left heel hurt—does side matter?
Short answer: side matters because loading matters. Road camber typically tilts to the right in right‑hand‑traffic countries; running on the left side of the road means the right foot sits slightly lower, absorbing more impact. On out‑and‑back routes done on the same roadway edge, one heel can be over‑loaded run after run. Track direction (counter‑clockwise) can likewise bias the left leg on curves.
Subtle leg‑length discrepancy (true or functional), prior ankle sprain on one side, or hip/core weakness can shift load. Footwear can nudge things, too: a higher heel‑to‑toe drop (e.g., 8–12 mm / ~0.3–0.5 in) may soothe the Achilles but increase plantar fascia tension for some runners, while lower‑drop shoes may do the opposite. Translation: if one heel complains, examine route camber, turn bias, and shoe specs before blaming fate. Don’t sleep on gait retraining—small cadence and posture tweaks can de‑stress the cranky side.
How do clinicians confirm the diagnosis?
Short answer: history and exam lead, imaging clarifies when needed. A sports‑minded clinician will palpate specific zones of the heel, assess ankle dorsiflexion, evaluate tibial/tarsal rotation, and look at single‑leg squat mechanics. If red flags or atypical features arise (night pain, swelling, neurologic symptoms, or persistent pain despite care), imaging enters the chat.
Common diagnostic tools (with typical utility and U.S. cash‑pay ranges):
| Method | How it’s done | Clinical utility (1–10) | Typical U.S. price range |
|---|---|---|---|
| X‑ray (foot/heel views) | Quick radiographs to look for fractures, alignment, and large heel spurs (spurs aren’t the pain source in most runners). | 6 | ~$150–$350 per series ⧉ |
| Ultrasound (high‑frequency, dynamic) | Real‑time view of plantar fascia thickness/degeneration, bursae, tendon neovascularity; guides injections precisely. No radiation. | 8 | ~$200–$600, depending on region and depth |
| MRI (foot/ankle) | Gold‑standard view of fascia, bone marrow edema (stress injury), bursae, nerves. Helpful when diagnosis is unclear or surgery is considered. | 9 | ~$750–$1,500 typical (national averages span wider) |
| CT | Detailed bone assessment when complex fracture is suspected. | 7–9 | ~$400–$1,500 depending on protocol |
Ultrasound pearls: in experienced hands it can measure plantar fascia thickness (>4.0 mm often correlates with symptoms), spot partial tears, and guide precise injections or fenestration. Reyus Mammadli, medical consultant, notes that ultrasound‑guided procedures “strike a sweet spot of accuracy, comfort, and cost efficiency for many runners.”
What at‑home steps actually help (and which are a hard no)?
Short answer: load management + targeted mobility/strength + footwear tweaks. That’s the trifecta.
- Relative rest and cold therapy: reduce run volume and vertical gain temporarily; use a cold pack for 15–20 minutes (32–40 °F / 0–4 °C) after runs.
- Stretch what’s tight: twice‑daily calf and plantar fascia stretching (30–45 seconds × 3–5 reps) and gentle rolling on a lacrosse ball or frozen water bottle. Progressive eccentric calf work (straight‑ and bent‑knee heel drops) helps the Achilles‑plantar fascia complex.
- Night positioning: a soft night splint (e.g., Strassburg Sock or Bird & Cronin posterior splint) keeps the fascia on a mild stretch to reduce first‑step pain.
- Footwear and inserts: temporarily favor models with more cushioning and moderate drop (8–12 mm / ~0.3–0.5 in). Consider quality over‑the‑counter orthoses from Superfeet, PowerStep, or Vasyli; custom devices when needed.
- Taping: low‑dye or kinesiology taping can offload the fascia for key workouts.
What’s a hard no? Jumping straight into aggressive hill repeats, ignoring morning pain, or doing ballistic calf stretches. The 2023 guideline emphasizes progressive loading, stretching, and patient‑specific education as first‑line care ⧉.
Risk‑Reduction Strategies for Runners with Heel Pain
Relative reduction shown as percent (%). Bars keep a minimum visual width for readability; badges show exact or mid‑range estimates.
Shoe rotation (alternate 2+ models)
39%What & why: Switching between different midsoles/geometry changes how forces hit the heel across days, cutting repetitive stress hot‑spots. How: keep two trainers with distinct cushioning/rocker; alternate daily (≈50/50). Track mileage per pair to avoid overusing one.
Increase cadence by 5–10%
~12%What & why: A modest step‑rate bump shortens overstride and lowers impact loading rates linked to heel/Achilles irritation. How: use a metronome or tempo playlist; e.g., 165 → 175 spm on easy runs. Keep posture tall, let speed stay easy while adapting.
Replace shoes every 300–500 miles (480–800 km)
~18%What & why: Packed‑out foam rebounds less and shifts force to the heel/arch; timely replacement stabilizes load. How: log mileage; check for flattened midsoles, new hot‑spots, or loss of “snap.” Rotate pairs so each gets recovery time.
Mix route camber & surfaces
~10%What & why: Repeating the same cambered road loads one heel more. Varying camber and terrain spreads stress and calms flares. How: alternate road sides on out‑and‑backs; add flat paths/track/treadmill 1–2× weekly; avoid steep camber on recovery days.
Use values as comparative guides; exact effects vary with training load, history, and mechanics.
Source: iytmed.com
Which clinic treatments are worth it?
Short answer: several modern options help once basics are dialed. Evidence has matured.
- Extracorporeal Shockwave Therapy (ESWT): Focused or radial shockwaves stimulate healing in chronic plantar fasciopathy. Meta‑analyses show superior mid‑term pain relief and function versus corticosteroid injections in chronic cases ⧉. Typical protocol: 3–5 sessions, weekly, with devices such as EMS Swiss DolorClast or Dornier systems. Expect temporary soreness, then gradual improvement over 4–12 weeks.
- Platelet‑Rich Plasma (PRP): Autologous platelet concentrate injected under ultrasound guidance to modulate healing. Recent systematic reviews suggest PRP can provide longer‑term benefit than corticosteroid for chronic plantar fasciopathy, though protocols vary ⧉.
- Corticosteroid injections: May give short‑term relief (weeks), but repeated doses risk fascia weakening or fat‑pad atrophy. Best used sparingly and under ultrasound guidance.
- Minimally invasive procedures: Percutaneous ultrasonic tenotomy (e.g., Tenex/TenJet) or radiofrequency microtenotomy (Topaz) are options when months of conservative care fail. These micro‑debridement techniques target degenerative fibers while sparing healthy tissue; recovery usually involves a short boot period and graded return to running.
Reyus Mammadli, medical consultant, often recommends ESWT first for runners who have plateaued after 8–12 weeks of solid home therapy: “It preserves tissue, gets people back faster, and plays nicely with gait and shoe adjustments.”
What do real‑world cases look like?
Short answer: heel pain stories vary, but patterns repeat.
- Female, 42, Denver, CO: Left heel pain after marathon build. Exam consistent with plantar fasciopathy; ultrasound thickness 5.2 mm. After 8 weeks of progressive loading, night splinting, and a switch to a cushioned trainer, pain plateaued. Three sessions of focused ESWT plus custom orthoses reduced morning pain from 7/10 to 2/10; running resumed at 8 weeks post‑ESWT.
- Male, 35, Austin, TX: Right posterior heel ache during tempo days; visible tendon thickening. Diagnosis: mid‑portion Achilles tendinopathy. Eccentric program + cadence cueing (from 164 to ~174 steps/min) and a temporary shoe with 10 mm (~0.39 in) drop led to steady gains; added radial ESWT at week 6. Pain‑free strides by week 10.
- Female, 55, Orlando, FL: Bilateral heel burning with tight shoes; worse at day’s end. Nerve entrapment suspected; improved with wider toe box shoes, nerve‑glide exercises, and ultrasound‑guided hydrodissection of Baxter’s nerve. Back to 5K jog‑walk within a month.
What about shoes, inserts, and surfaces—how much do they matter?
Short answer: a lot. Cushioning, geometry, and rotation influence load.
- Cushioning & geometry: higher stack shoes (e.g., HOKA Clifton, ASICS Gel‑Nimbus, Brooks Glycerin) can soften impact on hard routes, while moderate drop (8–12 mm / ~0.3–0.5 in) may help calm the Achilles‑plantar complex during flares. Rocker soles ease forefoot loading and can reduce peak plantar pressures.
- Inserts: quality prefabricated orthoses often rival custom devices early on and are easier to swap between shoes.
- Rotation: using more than one model spreads repetitive stress; prospective data suggest runners who rotate shoes cut injury risk substantially during a 22‑week season ⧉.
- Surfaces & routes: alternate cambered roads with flat paths, tracks, treadmills, or trails. Replace shoes every ~300–500 miles (480–800 km) or when midsole rebound is clearly reduced.
Here’s the deal: the “perfect shoe” is the one that matches a runner’s load tolerance and mechanics today—it can change across a training cycle. That’s normal.
When should a runner seek medical care quickly?
Short answer: sooner rather than later if red flags show up.
- Pain persists beyond 2–3 weeks despite down‑shifting mileage and diligent home care.
- Pain at rest/night, progressive swelling, numbness/tingling, or inability to bear weight.
- Focal bony tenderness after a mileage spike (think stress reaction/fracture) or a sudden pop in the calf/heel.
- Recurrent flares with every attempt to rebuild—time to audit gait, route camber, and footwear with a clinician.
Achilles tendon issues are common in active populations; among recreational runners, incidence during a season can reach single‑digit percentages, and elite groups report much higher burdens, underscoring the need to address calf strength and loading strategy early .
Practical tables runners actually use
A. Diagnostic choice at a glance
| Scenario | First‑line | Consider next | Why |
|---|---|---|---|
| Classic first‑step pain, normal exam otherwise | Ultrasound in clinic | MRI if non‑responsive | Ultrasound confirms thickened fascia, guides therapy; MRI if stress injury suspected. |
| Focal bony heel pain after rapid mileage jump | X‑ray | MRI | X‑ray may miss early stress injury; MRI shows marrow edema. |
| Posterior heel swelling/tenderness | Ultrasound | — | Distinguish Achilles tendinopathy vs bursitis; guide injections if needed. |
| Atypical burning/tingling | Exam + ultrasound | Nerve conduction study | Rule out Baxter’s nerve entrapment; consider hydrodissection. |
B. Treatment ladder & expected timeline
| Time frame | Focus | What success looks like |
|---|---|---|
| Weeks 0–2 | Load dial‑down, cold therapy, taping, shoe tweak | Morning pain intensity drops; fewer post‑run zingers. |
| Weeks 2–6 | Calf/fascia mobility, progressive loading, night splint | Longer pain‑free walking; easy runs return. |
| Weeks 6–12 | Add ESWT or PRP if plateau; refine gait and shoe rotation | Sustained improvement in first‑step pain; workouts rebuild. |
| Beyond 12 weeks | Consider minimally invasive options if function stalls | Targeted procedures with guided rehab; return to races. |
Editorial Advice
Reyus Mammadli, medical consultant, emphasizes a principle‑first approach: “Match the runner’s current tissue capacity with the day’s load, then build slowly. Tools like ESWT or PRP work best on top of disciplined loading and shoe strategy.” The editorial team adds:
- Use a small route audit: if one heel hurts, flip road sides on out‑and‑backs, add flat routes twice per week, and cap single‑run ascent early in rehab.
- Keep a two‑shoe rotation (different midsoles/geometry) during base building; it’s low effort, high reward for load variability.
- For hot spots, a temporary heel lift (5–8 mm / 0.2–0.3 in) inside the trainer can calm the Achilles‑plantar unit while strength work catches up.
- If morning pain is >5/10 for a week, that’s a nudge to scale back. That’s a hard no on racing through it.