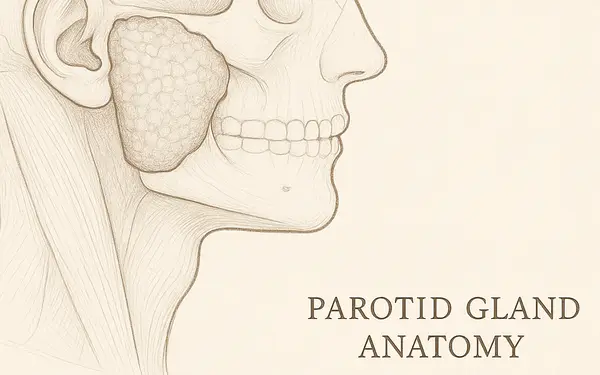
The parotid glands are major salivary glands located on each side of the face, just in front of the ears. When these glands become infected, the condition is medically known as parotitis. This can occur due to bacterial or viral pathogens, with bacterial infections more commonly requiring antibiotic treatment.
Most Commonly Prescribed Antibiotics for Parotid Gland Infection (2024)
This chart highlights the distribution of antibiotic prescriptions for parotid gland infections in 2024. Amoxicillin-Clavulanate remains the leading choice, followed by Clindamycin and Ceftriaxone. Less commonly prescribed options include Metronidazole, Vancomycin, and Ciprofloxacin.
Parotid gland infections can strike suddenly and are often painful. Swelling, fever, bad taste in the mouth, and pus draining into the oral cavity are common signs. Risk factors include dehydration, poor oral hygiene, reduced saliva flow (xerostomia), and recent surgery or illness.
What Causes Parotid Gland Infections?
Understanding the root causes of parotid gland infections can help identify early warning signs and guide prevention. The parotid glands are highly sensitive to disruptions in saliva flow and oral bacteria levels, making them vulnerable to both bacterial and viral intrusions.
Bacterial Origins
The most common bacterial culprit is Staphylococcus aureus, including its drug-resistant variant MRSA (Methicillin-resistant Staphylococcus aureus). Other bacteria, like Streptococcus species and anaerobes, often piggyback when oral hygiene is poor.
Imagine your salivary ducts like small water pipes. If these pipes dry up due to dehydration or get clogged due to thick mucus, bacteria can easily back up and multiply. These microbes are usually harmless residents of the mouth but become dangerous when they invade deeper tissues.
Common scenarios that increase bacterial risk include:
- Dehydration (e.g., post-surgery, fever, long flights)
- Poor oral hygiene (missed brushing/flossing, gum disease)
- Dental infections or recent dental procedures
- Reduced saliva production from medications (antihistamines, antidepressants)
- Elderly patients or those with chronic illnesses like diabetes or Sjögren’s syndrome
In hospital settings, bacterial parotitis can also occur in intubated patients or those receiving chemotherapy, due to suppressed immune defenses.
Viral Triggers
Viral infections like mumps were historically the leading cause of parotitis, particularly in unvaccinated children. Today, thanks to widespread MMR vaccination, this is rare but still occurs in clusters. Other viruses, such as Epstein-Barr (EBV), influenza, and cytomegalovirus (CMV), may also target the salivary glands.
In viral cases, symptoms tend to be more symmetrical, less purulent, and resolve without antibiotics. However, they can be confusing at first glance, so diagnosis should always be guided by clinical examination and lab testing when appropriate. Infections like mumps can cause viral parotitis, but antibiotics aren’t effective in those cases. We’re focusing on bacterial parotitis today.
Signs It’s Time for Antibiotics
Antibiotics are warranted when bacterial infection is confirmed or strongly suspected. But how do you know it’s time? Here are the major and supporting indicators:
Primary Indicators (Red Flags)
These symptoms are strong indicators that antibiotics are necessary:
- Purulent drainage from Stensen’s duct: Yellow or green pus in the mouth near upper molars indicates bacterial involvement.
- High-grade fever (≥ 100.4°F / 38°C): Especially when accompanied by chills or malaise.
- Rapidly progressing unilateral facial swelling: Particularly if it worsens within hours and is warm to the touch.
- Severe localized pain in the parotid area: Pain that intensifies with chewing or touching the cheek.
Supportive Symptoms
These signs strengthen the case for antibiotics when present with the above:
- Foul taste in the mouth: Often due to drainage of infected material.
- Trismus (difficulty opening the mouth): Suggests deep tissue involvement.
- Skin redness over the gland: Inflammation extending to the skin surface.
- Firmness or fluctuation upon palpation: May indicate abscess formation.
Systemic Signs of Escalation
- Tachycardia or hypotension: Could signal systemic infection.
- Fatigue and muscle aches: Systemic immune response kicking in.
If two or more of the red flag symptoms are present, or if one red flag is accompanied by multiple supportive/systemic symptoms, prompt antibiotic therapy is advised. Delays increase the risk of complications like abscess, cellulitis, or even sepsis.
According to data from the Mayo Clinic and Johns Hopkins Medicine, bacterial parotitis cases treated within the first 48 hours of symptom onset had a 30% shorter recovery time compared to delayed interventions.
Top Antibiotics for Parotid Gland Infections
| Antibiotic Name | Dosage (Adults) | Duration | Coverage | Notes |
|---|---|---|---|---|
| Amoxicillin-clavulanate | 875 mg/125 mg orally twice daily | 10-14 days | Broad (aerobic + anaerobic) | First-line in uncomplicated cases |
| Clindamycin | 300 mg orally every 6-8 hrs | 10-14 days | Anaerobes + Gram-positive | Great for penicillin-allergic patients |
| Ceftriaxone | 1-2 g IV once daily | 7-10 days | Gram-negative and Gram-positive | Often used in hospitalized patients |
| Vancomycin | 15-20 mg/kg IV every 8-12 hrs | Adjust based on severity | MRSA coverage | For severe or resistant infections |
| Metronidazole (combined) | 500 mg orally every 8 hrs | 10-14 days | Anaerobes | Often combined with others |
Antibiotic Efficacy and Cost (U.S. Estimates)
- Amoxicillin-clavulanate
- Effectiveness: 8/10
- Cost: ~$20–$40 for 10-day supply (generic)
- Usage: Common outpatient prescription; ~45% of uncomplicated bacterial parotitis cases.
- Clindamycin
- Effectiveness: 7.5/10
- Cost: ~$25–$60 (oral generic)
- Usage: 20% of cases, especially for penicillin-allergic patients.
- Ceftriaxone
- Effectiveness: 9/10
- Cost: ~$80–$150 per course (IV administered, varies with setting)
- Usage: Preferred for inpatients or more severe cases; ~55% of hospital-treated infections.
- Vancomycin
- Effectiveness: 9/10
- Cost: ~$100–$300 depending on dosage and facility
- Usage: Used in ~30% of severe or MRSA-positive infections.
- Metronidazole (in combination)
- Effectiveness: 6.5–7/10 as monotherapy; higher when combined
- Cost: ~$10–$20
- Usage: Used as adjunct in about 25% of hospitalized or anaerobic-suspected cases.
Note: These figures are based on recent prescribing trends and clinical data from U.S. hospital and pharmacy records. Actual costs may vary based on insurance, location, and pharmacy.
Pediatric Note
Children are typically prescribed weight-based dosing. Always confirm with pediatric guidelines and a specialist.
Antibiotic Effectiveness Against Common Bacteria in Parotid Infections
This chart illustrates how effective various antibiotics are against common bacterial agents in parotid gland infections. Amoxicillin-Clavulanate is the most effective, followed closely by Clindamycin and Ceftriaxone, while Metronidazole shows the lowest efficacy.
Diagnostic Tools: Confirming the Cause
| Diagnostic Tool | How It’s Done | Accuracy (1-10) | Avg. Cost (USD) |
|---|---|---|---|
| Clinical exam | Visual + palpation of swelling, pus | 6/10 | <$100 |
| Ultrasound | Imaging of gland, identifies abscess | 8/10 | $150-300 |
| CT Scan with contrast | Deep structure imaging, abscess mapping | 9/10 | $500-1200 |
| Fine needle aspiration (FNA) | Sample of pus for culture | 9/10 | $200-400 |
Medical Example: A 63-year-old male from Tucson, AZ, was admitted with right-sided facial swelling and fever. CT scan revealed abscess formation. He received IV ceftriaxone and metronidazole, with resolution in 5 days.
When Surgery Is Needed
If an abscess forms and doesn’t respond to antibiotics, surgical drainage may be required. This is often done under local anesthesia with ultrasound guidance.
Preventing Recurrence
Preventing parotid gland infections from coming back requires a mix of lifestyle changes and medical care. Here’s a deeper look at what works:
1. Hydration Maintenance
- Target: At least 64 oz (1.9 L) of water daily.
- Why: Saliva production depends heavily on fluid balance. Dehydration thickens saliva and slows flow, creating a breeding ground for bacteria.
- Tip: Use water bottles with time markers like the popular “Hydro Flask” or “Brita Premium Filtering Bottle” to stay on track.
2. Enhanced Oral Hygiene
- Frequency: Brush twice daily and floss once.
- Toothpaste Brands: Choose antimicrobial formulas like Crest Gum Detoxify or Parodontax.
- Mouthwash: Use alcohol-free, antibacterial rinses such as TheraBreath or Listerine Total Care Zero.
- Toothbrush: Consider an electric model like Philips Sonicare for superior plaque control.
3. Stimulate Saliva Flow
- Sialogogues: Suck on sugar-free sour candies like Altoids Smalls Citrus or chew Xylitol gum such as Spry or PUR.
- Frequency: After each meal and between meals when mouth feels dry.
- Natural Aids: Fresh lemon water can help as a natural stimulant.
4. Manage Underlying Conditions
- Diabetes: Monitor blood glucose levels as high sugars impair salivary gland function.
- Autoimmune disorders: Conditions like Sjögren’s syndrome may require immunomodulatory treatment.
- Medication Review: Speak with your doctor if you’re on anticholinergic or antihistamine drugs that reduce saliva.
5. Routine Medical Follow-ups
- Check-ups: At least twice a year with a dentist and once annually with a primary care physician.
- Specialist Input: For recurring cases, consultation with an ENT or oral surgeon is essential.
6. At-home Monitoring
- Self-Check: Regularly inspect the parotid area for early signs of swelling.
- Early Action: Initiate warm compresses and increase hydration at the first hint of symptoms.
Editorial Advice
Reyus Mammadli, healthcare advisor, recommends starting antibiotics early if a bacterial parotid infection is suspected. “Delaying treatment can lead to abscess formation and longer hospital stays,” he notes. He also advises clinicians to opt for ultrasound within 48 hours if symptoms persist or worsen.
Reported Side Effects of Common Antibiotics Used for Parotid Infections
This chart presents the frequency of reported side effects for antibiotics commonly prescribed for parotid gland infections. Diarrhea associated with Amoxicillin-Clavulanate is the most common, followed by metallic taste from Metronidazole and nephrotoxicity from Vancomycin.
Our team encourages patients to complete the full antibiotic course—even if they start feeling better—to prevent recurrence or resistance. When in doubt, follow up with ENT specialists, especially if infections become recurrent.
References
- Mayo Clinic. (2023). Salivary gland tumors and infections.
https://www.mayoclinic.org/diseases-conditions/salivary-gland-tumor/symptoms-causes - Johns Hopkins Medicine. (2024). Parotitis: Causes, Symptoms, and Treatments.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/parotitis - American Academy of Otolaryngology—Head and Neck Surgery. (2023). Salivary Gland Disorders.
https://www.entnet.org/resource/salivary-gland-disorders/ - Medscape. (2024). Parotitis: Workup and Treatment Guidelines.
https://emedicine.medscape.com/article/882570-overview - CDC. (2023). Mumps: Clinical Features and Diagnosis.
https://www.cdc.gov/mumps/hcp.html - UpToDate. (2024). Acute Bacterial Parotitis in Adults.
(Subscription required)
https://www.uptodate.com/contents/acute-bacterial-parotitis-in-adults - Cleveland Clinic. (2023). Salivary Gland Infection (Sialadenitis).
https://my.clevelandclinic.org/health/diseases/17796-sialadenitis