Experiencing unexpected bleeding between periods can be unsettling, especially if it comes with cramps. While sometimes the cause is harmless, in other cases it may point to a health issue that needs attention. Understanding why this happens, how it is diagnosed, and what treatments are available can help women make informed decisions about their health.
How Common Are the Causes of Intermenstrual Bleeding?
Hormonal Fluctuations — 30%
Shifts from starting/stopping contraception or natural cycle changes can trigger mid-cycle spotting; Seriousness: usually mild and self-limited.
Fibroids & Polyps — 25%
Benign growths in the uterus or cervix that can irritate the lining and cause bleeding; Seriousness: typically moderate, often needs evaluation.
Ovulation Spotting — 20%
A brief mid-cycle bleed when the ovary releases an egg; Seriousness: mild and harmless unless pain is severe.
Endometriosis — 10%
Uterine-like tissue grows outside the uterus, causing inflammation, cramps, and spotting; Seriousness: moderate to high if symptoms persist.
Thyroid Disorders — 5%
An under- or overactive thyroid can disrupt cycle signals and lead to spotting; Seriousness: usually mild, treatable with medication.
Cancer or Precancer — 3%
Abnormal cells in the cervix or uterus can cause bleeding between periods; Seriousness: high—prompt medical assessment is essential.
Source: iytmed.com
What Is Intermenstrual Bleeding and Why Does It Matter?
Intermenstrual bleeding, also known as spotting or metrorrhagia, refers to vaginal bleeding that occurs outside of a regular menstrual cycle. Normally, a menstrual cycle lasts 21 to 35 days, with bleeding lasting about 5 days. The typical blood loss is around 30–80 ml (2–8 tablespoons). Any bleeding outside of this range is considered irregular.
This matters because unusual bleeding can sometimes be linked to benign conditions, such as fibroids or hormonal changes, but it can also be an early sign of more serious problems, including precancerous changes or cancer of the uterus or cervix. According to the American College of Obstetricians and Gynecologists (ACOG), about 10% of women with postmenopausal bleeding are later diagnosed with uterine cancer ⧉. This is why every instance of unexpected bleeding should be evaluated by a medical professional.
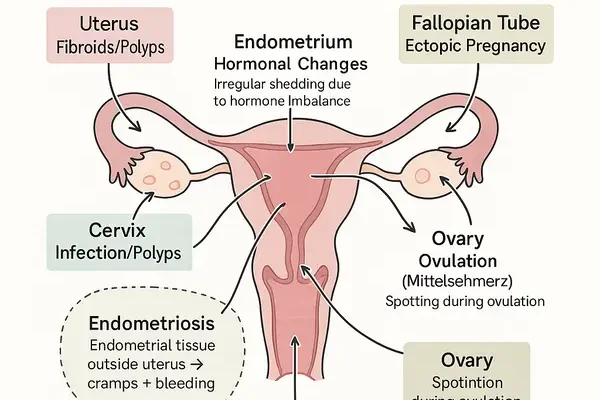
Typical Causes of Vaginal Bleeding Between Periods
There are many possible reasons why bleeding can occur between menstrual cycles. Below are the most common causes, explained in simple terms, along with how serious they may be:
- Hormonal fluctuations – Hormones are like the body’s internal “traffic lights” for the menstrual cycle. If levels rise or fall too quickly (for example, after starting, stopping, or missing birth control pills), the body can get “confused” and shed a little lining at the wrong time. Seriousness: usually mild, often improves with lifestyle changes or adjusting medication, but needs monitoring if persistent.
- Uterine fibroids or polyps – Think of these as small, non-cancerous “lumps” or “growths” inside the uterus or cervix. They can sometimes press on the uterine lining and cause extra bleeding. Seriousness: usually not dangerous, but can be uncomfortable and require removal if symptoms worsen.
- Ovulation spotting (Mittelschmerz) – Around mid-cycle, when the ovary releases an egg, some women notice light spotting or mild cramps. It’s a bit like a brief “signal” from the body that ovulation is happening. Seriousness: harmless and self-limiting, no treatment needed unless pain is severe.
- Pregnancy-related causes – Light bleeding can sometimes mean implantation (the embryo attaching to the uterus). But it may also point to miscarriage or ectopic pregnancy (when the embryo grows outside the uterus). Seriousness: ranges from mild to urgent. Implantation bleeding is harmless, but ectopic pregnancy is a medical emergency.
- Infections or inflammation – If the cervix becomes irritated by bacteria, viruses, or sexually transmitted infections, it can bleed easily. It’s similar to how gums bleed when inflamed. Seriousness: needs treatment, usually antibiotics or antivirals, since leaving infections untreated may cause complications.
- Endometriosis – In this condition, the tissue that normally lines the uterus grows in the wrong place (outside the uterus). Imagine “wallpaper” peeling and sticking to the wrong wall—it causes irritation, cramps, and spotting. Seriousness: chronic but manageable with medication or surgery.
- Thyroid disorders – The thyroid is like the body’s “thermostat” for hormones. If it’s underactive, it can throw off the menstrual cycle and lead to spotting. Seriousness: usually mild, controlled with thyroid medication and lifestyle adjustments.
- Certain medications – Blood thinners (like warfarin) can make bleeding heavier or more frequent, even outside of periods. Seriousness: depends on dose and monitoring; not usually dangerous if managed correctly.
- Cancer or precancer – Rarely, bleeding between periods is linked to cancers of the cervix, uterus, or endometrium. Think of this as the body’s “warning alarm” that something more serious may be happening. Seriousness: high—requires immediate evaluation by a doctor.
Reyus Mammadli, medical consultant, notes that explaining the seriousness of each possible cause helps women respond appropriately—whether that means reassurance and watchful waiting or urgent medical care.
When Cramps Join the Picture: What It May Indicate
Cramping between periods often raises concern because it suggests the uterus is actively contracting outside of normal menstruation. The most common explanations include:
- Pregnancy – Implantation can cause mild cramps with light bleeding, while ectopic pregnancy may cause sharper pain and requires urgent medical care.
- Endometriosis or adenomyosis – Chronic conditions where uterine tissue grows outside or deep within the uterine wall, causing painful cramps and spotting.
- Ovulation pain (Mittelschmerz) – Usually short-lived and not harmful.
A case reported from New York: a 29-year-old woman experienced persistent mid-cycle cramps and spotting. After an ultrasound and laparoscopy, she was diagnosed with endometriosis, which explained both symptoms.
Real-Life Cases from U.S. Women
Case 1: Maria, 42, from Texas – Living with Fibroids
Maria had been noticing heavy spotting and cramps for almost a year. At first, she thought it was just stress or age catching up with her. But when she began needing to change pads every two hours, she realized it wasn’t normal. After a pelvic ultrasound, doctors found fibroids in her uterus. She underwent a laparoscopic myomectomy, a minimally invasive surgery, and was back on her feet in two weeks. For Maria, finally having an explanation and a solution was a huge relief.
Case 2: Jennifer, 35, from California – A Polyp That Wouldn’t Be Ignored
Jennifer noticed light bleeding after intimacy and sometimes in the middle of her cycle. It lasted for several months, and she worried something serious was wrong. A gynecologist performed a hysteroscopy and discovered a cervical polyp. The outpatient procedure to remove it took less than an hour, and she was back at work the next day. Jennifer says she now pays much closer attention to her cycle and feels empowered knowing the cause was treatable.
Case 3: Ashley, 29, from New York – Struggling with Endometriosis
Ashley had dealt with unpredictable mid-cycle cramps and bleeding since her early twenties. At first, doctors told her it might just be “bad periods.” But when the pain became so severe it interfered with her job, she sought out a specialist. A laparoscopy confirmed endometriosis. She had excision surgery followed by hormone therapy, and while she still has occasional flare-ups, she says her quality of life has improved dramatically. Ashley’s story shows that persistence and seeking expert care can lead to real answers.
These cases illustrate the variety of causes behind intermenstrual bleeding and highlight the importance of taking symptoms seriously, no matter how common or minor they may seem at first.
How Doctors Diagnose Intermenstrual Bleeding Today
Modern diagnostics combine traditional exams with advanced imaging and lab tests:
- Pelvic ultrasound – Non-invasive, high accuracy (8/10), average cost: $200–$500.
- Transvaginal 3D ultrasound – Offers detailed imaging (9/10), cost: $400–$800.
- Hysteroscopy – A tiny camera inserted into the uterus for direct visualization (accuracy 9/10), cost: $1,000–$3,000.
- Endometrial biopsy – Tissue sampling for cancer screening (accuracy 8/10), cost: $300–$800.
- Pap smear and HPV testing – For cervical health (accuracy 7/10), cost: $50–$150.
- Blood tests – For thyroid function and hormone levels (accuracy 7/10), cost: $100–$300.
Accuracy of Diagnostic Methods
Transvaginal 3D Ultrasound — 9/10
A slim probe is inserted into the vagina to capture detailed 3D images of the uterus and ovaries. Results are immediate, viewed during the exam.
Hysteroscopy — 9/10
A thin camera is gently passed through the cervix into the uterus, allowing direct visualization. Results are immediate during the procedure.
Endometrial Biopsy — 8/10
A thin tube is inserted through the cervix to collect a sample of the uterine lining. Results usually available in 2–5 days after lab analysis.
Pap Smear + HPV Test — 7/10
Cells are gently scraped from the cervix with a small brush or spatula. Results are usually ready within several days to one week.
Blood Tests — 7/10
Blood is drawn from a vein to measure thyroid hormones and reproductive markers. Results typically available within 24 hours to a few days.
Pelvic Ultrasound — 8/10
A probe is moved across the lower abdomen with gel to create images of pelvic organs. Results are immediate, visible during the scan.
Source: iytmed.com
According to Cleveland Clinic experts, hysteroscopy combined with biopsy remains the gold standard for identifying precancerous changes ⧉. Meanwhile, non-invasive ultrasounds are often used first due to accessibility and affordability.
Treatment Options: From Medications to Modern Procedures
Medications
Medications are often the first step when intermenstrual bleeding is linked to hormonal imbalance or inflammation. Commonly prescribed options include:
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Ibuprofen (Advil, Motrin) is widely used to relieve pain and decrease menstrual blood flow. Effectiveness: 6/10. Average cost: $10–$20 per month. Popular as a short-term, over-the-counter solution.
- Hormonal Birth Control Pills: Brands like Yaz, Ortho Tri-Cyclen, and Seasonale help regulate cycles and reduce spotting. Treatment duration: often long-term. Effectiveness: 8/10. Average cost: $15–$50 per month depending on insurance coverage. This remains one of the most common treatments among women in the U.S.
- Hormonal IUDs (Intrauterine Devices): Mirena and Kyleena release progestin to thin the uterine lining and reduce bleeding. Duration: effective for 3–5 years. Effectiveness: 9/10. Cost: $800–$1,200 upfront, but cost-effective long term. Increasingly popular due to convenience and dual role as contraception.
Surgical Interventions
Surgery is recommended when structural issues like fibroids or polyps are the cause.
- Myomectomy (Fibroid Removal): Minimally invasive laparoscopic techniques are common. Recovery: about 1–2 weeks. Effectiveness: 8/10. Cost: $5,000–$10,000. Considered a gold-standard treatment for symptomatic fibroids.
- Polypectomy (Polyp Removal): Often done via hysteroscopy in an outpatient setting. Recovery: 1–3 days. Effectiveness: 9/10. Cost: $500–$1,000. Highly effective with minimal downtime.
- Endometrial Ablation: Removes or destroys the uterine lining to reduce bleeding. Best for women who no longer wish to conceive. Recovery: 3–5 days. Effectiveness: 8/10. Cost: $3,000–$7,000. Popular for women in their 40s with heavy or irregular bleeding.
Advanced Therapies for Endometriosis
Women with endometriosis often require specialized treatments:
- Laparoscopic Excision Surgery: Surgeons remove endometrial tissue using small incisions and cameras. Recovery: 1–2 weeks. Effectiveness: 9/10. Cost: $8,000–$15,000. This remains the most definitive treatment for severe endometriosis.
- Hormone Modulators: Drugs like Elagolix (Orilissa) lower estrogen levels to reduce endometrial growth. Treatment duration: 6–24 months. Effectiveness: 7/10. Cost: around $900 per month. While not as common as surgery, these are increasingly prescribed for women who prefer medical over surgical management.
Reyus Mammadli notes that minimally invasive procedures and long-acting therapies have dramatically improved quality of life for many women, offering safer and faster recovery compared to older methods.
At-Home Monitoring and What You Can Safely Do Yourself
While home care cannot replace medical evaluation, women can:
- Track cycle length and bleeding patterns in a journal or app.
- Note the number of pads or tampons used per day to estimate blood loss.
- Use NSAIDs like ibuprofen for cramp relief.
- Avoid aspirin, as it can increase bleeding.
The Mayo Clinic recommends that women seek care if bleeding is heavy enough to soak through one or more pads or tampons every hour for several hours ⧉. Self-monitoring helps doctors make faster, more accurate diagnoses.
When It’s Time to See a Doctor Without Delay
Seek urgent care if:
- Bleeding is very heavy or prolonged.
- There is bleeding after menopause.
- Bleeding is accompanied by dizziness, fainting, or severe abdominal pain.
- You suspect pregnancy and experience pain or spotting.
Red Flag Symptoms That Shouldn’t Be Ignored
Heavy Prolonged Bleeding — 40%
This means soaking through pads or tampons every hour for several hours, or bleeding that lasts a week or longer. Red flag: needs immediate evaluation.
Postmenopausal Bleeding — 25%
Any vaginal bleeding after menopause, even light spotting, is abnormal. Red flag: should always be checked for cancer or precancer changes.
Severe Cramps with Spotting — 20%
Pain that interferes with daily activities and is paired with bleeding outside of periods can signal endometriosis or adenomyosis. Red flag: seek medical advice.
Dizziness or Fainting with Bleeding — 10%
Lightheadedness or fainting means blood loss may be severe, affecting circulation. Red flag: emergency care is required.
Pregnancy with Spotting — 5%
Spotting in pregnancy may be harmless, but can also indicate miscarriage or ectopic pregnancy. Red flag: requires urgent medical evaluation.
Source: iytmed.com
The National Cancer Institute highlights that postmenopausal bleeding, even if light, should never be ignored ⧉. Quick evaluation can detect treatable issues early.
Prevention and Lifestyle Factors That Play a Role
Although not all cases are preventable, maintaining overall health helps reduce risks:
- Keeping a healthy body weight.
- Managing chronic conditions like thyroid disorders or diabetes.
- Regular gynecologic checkups.
- Following up on any irregular bleeding immediately.
Lifestyle cannot replace medical care, but it supports hormonal balance and overall reproductive health.
Editorial Advice
According to medical consultant Reyus Mammadli, women should approach intermenstrual bleeding as a signal—not necessarily a red flag, but never something to brush aside. The best course is to monitor patterns, keep records, and seek timely care. With today’s advanced diagnostic tools and minimally invasive treatments, most causes of intermenstrual bleeding are effectively managed.
Editorial team tip: Always listen to your body. If something feels off, it probably is. Seeking care early often makes the difference between a simple solution and a more complicated journey.