This disease also known as Wide-complex tachycardia; V tach; Tachycardia – ventricular. Ventricular tachycardia (VT) is a quick heart beat that starts in the lower chambers of the heart (ventricles).
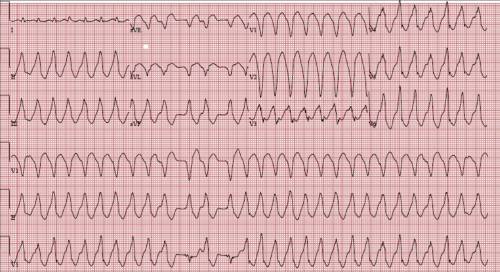
Monomorphic Ventricular Tachycardia
Ventricular Tachycardia (VT) is a broad complex tachycardia originating in the ventricles. There are several various varieties of VT– the most being Monomorphic VT.
Clinical Significance
- Ventricular tachycardia might hinder cardiac output with consequent hypotension, collapse, and intense cardiac failure. This is due to extreme heart rates and lack of coordinated atrial contraction (loss of “atrial kick”).
- The existence of pre-existing poor ventricular function is highly related to cardiovascular compromise.
- Reduced cardiac output might result in decreased myocardial perfusion with degeneration to VF.
- Prompt recognition and initiation of treatment (e.g. electrical cardioversion) is needed in all cases of VT.
Continual monomorphic ventricular tachycardia (SMVT) is specified by the following attributes:
- A regular wide QRS complex (≥ 120 milliseconds) tachycardia at a rate greater than 100 beats per minute
- The consecutive beats have a uniform and stable QRS morphology
- The arrhythmia lasts ≥ 30 seconds or causes hemodynamic collapse in <30 seconds.
ACLS Pulseless Ventricular Tachycardia
The pulseless ventricular tachycardia rhythm is mainly recognized by numerous requirements. First, the rate is generally higher than 180 beats per minute and the rhythm typically has a really large QRS complex.
Second, the patient will be pulseless and third, the rhythm comes from the ventricles. This remains in contrast to other types of tachycardias which have origination above the ventricular tissue (in the atria).
Not all ventricular tachycardias are pulseless and for that reason, pulselessness needs to be established prior to starting an algorithm. This is achieved merely by inspecting a carotid or femoral pulse.
Pulselessness with a tachyarrhythmia occurs due to the fact that the ventricles are not successfully moving blood from the heart and there is therefor no cardiac output. Many tachyarrhythmias of a rate > 150 will weaken into pulselessness if timely treatment is not given.
Pulseless ventricular tachycardia is treated using the left branch of the heart attack arrest algorithm.
Polymorphic Ventricular Tachycardia
Polymorphic ventricular tachycardia (PVT) is a type of ventricular tachycardia in which there are several ventricular foci with the resultant QRS complexes differing in amplitude, axis and period. The commonest reason for PVT is myocardial ischaemia.
Torsades de pointes (TdP) is a specific form of polymorphic ventricular tachycardia occurring in the context of QT prolongation; it has a particular morphology in which the QRS complexes “twist” around the isoelectric line.
For TdP to be diagnosed, the patient has to have evidence of both PVT and QT prolongation. Bidirectional VT is another type of polymorphic VT, most frequently connected with digoxin toxicity.
Supra Ventricular Tachycardia
Supraventricular tachycardia (SVT) implies that from time to time your heart beats very quickly for a reason aside from workout, high fever, or stress.
For many people who have SVT, the heart still works typically to pump blood through the body. Types of SVT include:
- Atrioventricular nodal reentrant tachycardia (AVNRT).
- Atrioventricular reciprocating tachycardia (AVRT), including Wolff-Parkinson-White syndrome.
During an episode of SVT, the heart’s electrical system doesn’t work right, triggering the heart to beat very fast. The heart beats a minimum of 100 beats a minute and may reach 300 beats a minute. After treatment or by itself, the heart normally returns to a normal rate of 60 to 100 beats a minute.
SVT might begin and end rapidly, and you might not have symptoms. SVT ends up being an issue when it occurs typically, lasts a long period of time, or causes symptoms.
Causes of Ventricular Tachycardia
VT is a pulse rate of more than 100 beats per minute, with at least 3 irregular heartbeats in a row.
The condition can develop as an early or late complication of a heart attack. It might also happen in people with:
- Cardiomyopathy
- Heart failure
- Heart surgery
- Myocarditis
- Valvular heart disease
VT can occur without heart disease.
Scar tissue might form in the muscle of the ventricles days, months, or years after a cardiovascular disease. This can result in ventricular tachycardia.
VT can likewise be brought on by:
- Anti-arrhythmic drugs (used to treat an abnormal heart rhythm).
- Modifications in blood chemistry (such as a low potassium level).
- Changes in pH (acid-base).
- Absence of enough oxygen.
“Torsade de pointes” is a kind of VT. It is frequently due to congenital heart disease or making use of certain medications.
Symptoms of Ventricular Tachycardia
You might have symptoms if the heart rate during a VT episode is really fast or lasts longer than a few seconds. Symptoms might consist of:
- Chest pain (angina).
- Fainting (syncope).
- Dizziness or lightheadedness.
- Experience of feeling the heart beat (palpitations).
- Shortness of breath.
Symptoms may start and stop suddenly. In many cases, there are no symptoms.
Diagnosis
The health care company will search for:.
- Missing pulse.
- Loss of consciousness.
- Normal or low blood pressure.
- Quick pulse.
Tests that may be used to find ventricular tachycardia include:
- Holter monitor.
- ECG.
- Intracardiac electrophysiology study (EPS).
- Rhythm tracking with a loop recorder or device.
You may also have blood chemistries and other tests.
Treatment for Ventricular Tachycardia
Treatment depends upon the symptoms, and the kind of heart disorder.
If someone with VT remains in distress, they may need:
- CPR.
- Cardioversion (electrical shock).
- Medicines (such as lidocaine, procainamide, sotalol, or amiodarone) offered through a vein.
After an episode of VT, actions are taken to more episodes.
- Medicines taken by mouth might be required for long-lasting treatment. Nevertheless, these drugs may have severe side effects. They are being used less typically as other treatments are developed.
- A procedure to damage the heart tissue that is triggering the abnormal heartbeat (called ablation) might be done.
- An implantable cardioverter defibrillator (ICD) may be used. It is a device that identifies any lethal, fast heartbeat. This irregular heart beat is called an arrhythmia. If it happens, the ICD rapidly sends out an electrical shock to the heart to alter the rhythm back to normal. This is called defibrillation.
Outlook (Prognosis)
The result depends upon the heart condition and symptoms.
Possible Complications
Ventricular tachycardia may not cause symptoms in some individuals. Nevertheless, it can be fatal. It is a significant reason for unexpected cardiac death.
When to Contact a Medical Professional
Go to the emergency room or call the local emergency situation number (such as 911) if you have a rapid, irregular pulse; faint, or have chest pain. All of these might be signs of ventricular tachycardia.
Prevention of Ventricular Tachycardia
Sometimes, the disorder can not be avoided. In other cases, it can be prevented by dealing with heart issues and avoiding certain medications.