Wernicke-Korsakoff Syndrome (WKS) is a severe neurological disorder caused by a deficiency of thiamine (vitamin B1). It primarily affects the brain and nervous system, leading to cognitive impairment and memory loss. WKS is often associated with chronic alcohol misuse, but it can also result from malnutrition, eating disorders, and certain medical conditions that impair thiamine absorption.
Progression of Wernicke’s Encephalopathy to Korsakoff’s Psychosis
This chart illustrates the progression of untreated Wernicke’s Encephalopathy into Korsakoff’s Psychosis. The data shows a significant increase in the percentage of patients developing chronic symptoms over time, emphasizing the need for early intervention.
What Are the Symptoms of WKS?
Wernicke-Korsakoff Syndrome consists of two phases:
- Wernicke’s Encephalopathy – an acute neurological condition marked by:
- Confusion and mental disorientation – Patients may struggle to process basic information, respond slowly in conversations, or appear dazed and unresponsive. This symptom often mimics intoxication, leading to frequent misdiagnoses.
- Lack of muscle coordination (ataxia) – Individuals may exhibit an unsteady gait, stumble frequently, or have difficulty performing simple motor tasks such as holding a spoon or buttoning a shirt.
- Abnormal eye movements or vision problems (ophthalmoplegia, nystagmus) – This includes involuntary eye jerking, drooping eyelids, and difficulty tracking objects, making reading or focusing on a single point challenging.
- Hypothermia and low blood pressure in severe cases – Some patients experience dangerously low body temperatures and circulatory issues, leading to dizziness, fainting, or an overall state of lethargy.
- Korsakoff’s Psychosis – a chronic and irreversible condition that follows if Wernicke’s Encephalopathy is not treated promptly. Symptoms include:
- Severe memory loss (especially anterograde amnesia) – Patients struggle to retain new information, often forgetting conversations within minutes and requiring constant reminders for daily tasks. This memory deficit can lead to repeated questions or confusion about recent events.
- Confabulation (fabricating memories) – Individuals unconsciously fill in memory gaps with fabricated stories, often believing them to be true. For example, a patient may confidently describe attending a family gathering that never occurred.
- Hallucinations – Some patients experience visual or auditory hallucinations, perceiving objects or voices that are not present, further complicating their cognitive state and interactions with others.
- Difficulty learning new information – Even with rehabilitation efforts, many struggle to retain new skills or knowledge, making tasks such as using new technology or remembering names incredibly challenging.
Common Symptoms of Wernicke’s Encephalopathy
This chart highlights the frequency of symptoms observed in diagnosed cases of Wernicke’s Encephalopathy. Confusion is the most prevalent symptom, followed by ataxia and vision impairments, while hypothermia occurs in a smaller percentage of patients.
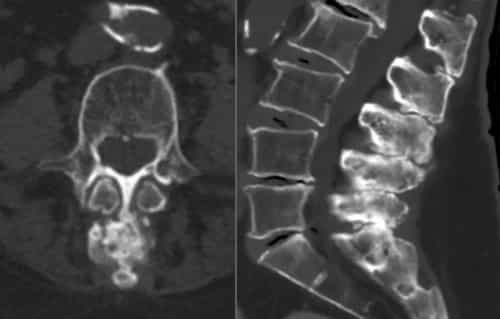
How is WKS Diagnosed?
Diagnosis is often challenging due to overlapping symptoms with other conditions like Alzheimer’s or stroke. The following methods help in identification:
| Diagnostic Method | Description | Accuracy (Scale 1-10) | Average Cost (U.S.) |
|---|---|---|---|
| Clinical Assessment | Neurological and psychiatric evaluation of symptoms | 6-7 | $200 – $500 |
| MRI & CT Scans | Detects brain damage in areas associated with WKS | 8-9 | $1,000 – $3,000 |
| Blood Tests & Vitamin Levels | Measures thiamine levels to confirm deficiency | 7-8 | $100 – $300 |
| Neuropsychological Testing | Evaluates cognitive impairment and memory issues | 7-9 | $500 – $1,500 |
What Are the Modern Treatment Options?
Treatment focuses on halting progression and preventing further damage. Key approaches include:
High-Dose Thiamine Therapy
Thiamine is administered intravenously in hospital settings, especially in acute cases, to rapidly replenish depleted levels. In less severe cases, oral supplements are prescribed. Patients often receive 500 mg intravenously for several days before transitioning to oral maintenance doses. Effectiveness: 8/10 – Works well when started early but does not reverse long-term damage.
Nutritional Support
Patients are encouraged to follow a diet rich in thiamine-containing foods such as whole grains, lean meats, and legumes. In some cases, dietary supplementation is required for life. Effectiveness: 7/10 – Helps prevent recurrence but requires strict adherence.
Alcohol Cessation Programs
Because alcohol abuse is a leading cause of WKS, strict and immediate cessation of alcohol consumption is essential. Patients must completely eliminate alcohol from their lives to prevent further neurological damage. Medical detoxification under professional supervision is recommended, followed by ongoing therapy to reinforce alcohol-free living. Some medications, such as naltrexone or acamprosate, may be prescribed to block alcohol’s effects and reduce cravings. Effectiveness: 8-10/10 – Highly effective when followed rigorously, though long-term success depends on the patient’s commitment to permanent sobriety.
Cognitive Therapy & Rehabilitation
Specialized cognitive rehabilitation programs focus on memory training, compensatory strategies, and task repetition to improve daily functioning. Patients may use notebooks or electronic reminders to manage their deficits. Effectiveness: 6/10 – Can enhance coping strategies but does not restore lost memories.
Pharmacological Support
Some studies suggest that medications like memantine (commonly used for Alzheimer’s) may help improve cognitive function in WKS patients, though research is still ongoing. Other drugs, such as donepezil, have been explored with mixed results. Effectiveness: 5-7/10 – Shows promise but lacks definitive proof.
Notable U.S. Medical Cases
- Male, 54, Texas – Diagnosed after long-term alcohol abuse. Recovered partially with intensive thiamine therapy but retained memory deficits.
- Female, 42, California – Developed WKS due to gastric bypass surgery complications. Early intervention helped full recovery.
- Male, 67, New York – Suffered severe Korsakoff’s psychosis; required permanent assisted living due to cognitive impairment.
Memory Loss Severity in Korsakoff’s Psychosis
| Memory Impairment Type | Percentage (%) |
|---|---|
| Anterograde Amnesia | 90% |
| Retrograde Amnesia | 70% |
| Confabulation | 65% |
This chart presents the severity of memory impairment in patients with Korsakoff’s Psychosis. Anterograde amnesia is the most prevalent, followed by retrograde amnesia and confabulation, highlighting the extensive cognitive impact of the condition.
Editorial Advice
Wernicke-Korsakoff Syndrome is a preventable and manageable condition when detected early. Reyus Mammadli, healthcare advisor, strongly emphasizes the necessity of routine health checkups for individuals at risk, particularly those with alcohol dependence or malnutrition. He categorically demands the complete and permanent avoidance of alcohol in any form, as its consumption directly contributes to the progression of WKS and other severe neurological conditions. Additionally, ensuring a diet rich in whole grains, legumes, and fortified cereals can help prevent thiamine deficiency. If you or someone you know exhibits symptoms, seeking immediate medical intervention can be life-changing.