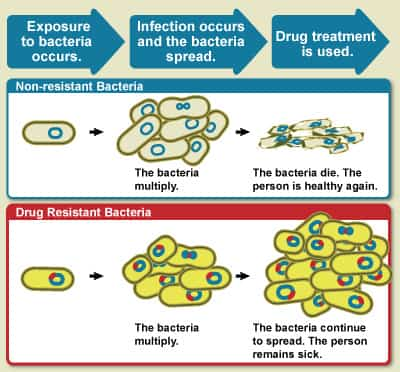
Antibiotic resistance occurs when an antibiotic has lost its ability to successfully control or kill bacterial growth; to puts it simply, the bacteria are “resistant” and continue to increase in the presence of restorative levels of an antibiotic.
Why Do Bacteria Become Resistant to Antibiotics?
Antibiotic resistance is a natural phenomenon. When an antibiotic is used, bacteria that can withstand that antibiotic have a greater chance of survival than those that are “susceptible.” Prone bacteria are killed or inhibited by an antibiotic, leading to a selective pressure for the survival of resistant pressures of bacteria.
Some resistance occurs without human action, as bacteria can produce and use antibiotics versus other bacteria, resulting in a low-level of natural choice for resistance to antibiotics. Nevertheless, the present higher-levels of antibiotic-resistant bacteria are attributed to the overuse and abuse of antibiotics. In some nations and over the Internet, antibiotics can be bought without a doctor’s prescription. Patients often take antibiotics unnecessarily, to treat viral illnesses like the common cold.
How Do Bacteria Become Resistant?
Some bacteria are naturally resistant to certain types of antibiotics. However, bacteria may also become resistant in two methods:
- by a hereditary anomaly or
- by obtaining resistance from another bacterium.
Mutations, uncommon spontaneous modifications of the bacteria’s genetic product, are believed to occur in about one in one million to one in 10 million cells. Various hereditary anomalies yield different types of resistance. Some mutations allow the bacteria to produce powerful chemicals (enzymes) that inactivate antibiotics, while other mutations get rid of the cell target that the antibiotic attacks. Still others close up the entry ports that enable antibiotics into the cell, and others produce pumping systems that export the antibiotic back outside so it never ever reaches its target.
Bacteria can get antibiotic resistance genes from other bacteria in numerous methods. By undergoing a basic breeding procedure called “conjugation,” bacteria can transfer hereditary product, consisting of genes encoding resistance to antibiotics (discovered on plasmids and transposons) from one bacterium to another. Viruses are another system for passing resistance characteristics between bacteria. The resistance qualities from one bacterium are packaged into the head part of the virus. The virus then injects the resistance qualities into any new bacteria it assaults. Bacteria likewise have the ability to acquire naked, “totally free” DNA from their environment.
Any bacteria that get resistance genes, whether by spontaneous anomaly or genetic exchange with other bacteria, have the ability to resist one or more antibiotics. Because bacteria can gather multiple resistance qualities with time, they can end up being resistant to many different families of antibiotics.
How Does Antibiotic Resistance Spread?
Genetically, antibiotic resistance spreads through bacteria populations both “vertically,” when new generations inherit antibiotic resistance genes, and “horizontally,” when bacteria share or exchange sections of genetic product with other bacteria. Horizontal gene transfer can even take place in between various bacterial types. Ecologically, antibiotic resistance spreads as bacteria themselves move from location to place; bacteria can travel through airplane, water and wind. People can pass the resistant bacteria to others; for example, by coughing or contact with unwashed hands.
Can Bacteria Lose Their Antibiotic Resistance?
Yes, antibiotic resistance characteristics can be lost, but this reverse procedure happens more gradually. If the selective pressure that is used by the existence of an antibiotic is removed, the bacterial population can possibly go back to a population of bacteria that reacts to antibiotics.
Prevention
5 ways to prevent antibiotic resistance:
- Understand that most of us do not need antibiotics for colds and influenza considering that they’re brought on by viruses
- Inform your doctor you just desire an antibiotic if it’s entirely needed
- Take the right dosage of your antibiotic at the right time, as prescribed by your doctor
- Only take your antibiotics for as long as your doctor tells you to
- From always washing your hands with warm soapy water to staying home whenever you’re sick, take steps to avoid infections and prevent them from spreading out.