It is crucial to maintain hydration and seek guidance from a healthcare provider if the symptoms continue or deteriorate.
How Does Taking Antibiotics Cause Diarrhea?
Are you curious about why taking antibiotics can sometimes lead to diarrhea? This how-to guide will provide you with a comprehensive explanation of this fascinating phenomenon. Although antibiotics are essential for treating bacterial infections, they can have some unwanted side effects, and diarrhea is one of them. So let’s dive in and discover the why behind this common occurrence.
Understanding the gut and its microbiome
In order to understand the connection between antibiotics and diarrhea, it is necessary to have a grasp on the gut and its microbiome. The gut consists of numerous beneficial bacteria that work together in harmony to carry out important tasks, including facilitating digestion, boosting the immune system, and preventing the growth of harmful bacteria.
How antibiotics work
Antibiotics are medications designed to kill or inhibit the growth of bacteria. They serve as a powerful tool in combatting bacterial infections, but unfortunately, their action is not selective. This means that in addition to targeting harmful bacteria causing the infection, antibiotics can also affect the beneficial bacteria residing in your gut.
Disrupting the balance
The use of antibiotics doesn’t just attack the bacteria that causes infections, but it also disrupts the natural balance of bacteria in the gut. Antibiotics cannot differentiate between beneficial and harmful bacteria, resulting in the destruction of both types. This disturbance can disturb the necessary balance for proper gut functioning.
Overgrowth of harmful bacteria or yeast
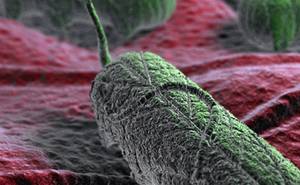
Due to the disruption caused by antibiotics, certain harmful bacteria or yeast, like Clostridium difficile (C. difficile), which is an opportunistic disease-causing microorganism, can exploit the weakened microbiome. These pathogens can rapidly multiply and generate toxins that cause irritation in the intestinal lining, resulting in diarrhea.
Altering bowel movements and digestion
Furthermore, the antibiotics’ impact on the gut microbiome can alter the pattern of bowel movements and digestion. These changes can cause symptoms like loose stools, increased frequency of bowel movements, abdominal discomfort, and bloating, which are commonly associated with antibiotic-induced diarrhea.
Duration and prevention
Antibiotic-induced diarrhea can occur during the course of treatment or even several weeks afterwards. It’s important to note that not everyone who takes antibiotics will experience diarrhea. The risk varies depending on the individual, the specific antibiotic used, and the overall health of their gut microbiome.
How to Recover Normal Intestinal Function in Diarrhea After Taking Antibiotics
Antibiotics are often prescribed to fight bacterial infections, but unfortunately, they can also disrupt the delicate balance of bacteria in our gut, leading to diarrhea. If you’re experiencing this side effect, don’t worry! There are steps you can take to restore your normal intestinal function. Here’s a helpful guide to get you back on track:
1. Stay Hydrated: Diarrhea can cause dehydration, so replenishing lost fluids and electrolytes is crucial. Drink plenty of water, herbal tea, clear broths, and consume rehydration solutions available at pharmacies. Avoid caffeine, as it can worsen diarrhea by stimulating the intestines.
2. Eat Gentle Foods: Stick to mild, easily digestible foods to give your gut a chance to heal. Opt for the BRAT diet: bananas, rice, applesauce, and toast. These foods are gentle on the stomach and can help firm up loose stools. Gradually introduce other bland foods like boiled potatoes, steamed vegetables, and lean protein.
3. Probiotics to the Rescue: Antibiotics eliminate both harmful and beneficial bacteria, which can disrupt the natural balance in your gut. Taking probiotics can help restore the friendly bacteria and promote a healthy digestive system. Look for supplements containing Lactobacillus and Bifidobacterium strains.
4. Fiber for Regularity: Incorporate more fiber into your diet to aid in restoring normal bowel movements. High-fiber foods like whole grains, fruits, vegetables, and legumes help bulk up the stool and regulate digestion. However, be cautious and start with small amounts, as too much fiber can aggravate diarrhea.
5. Avoid Trigger Foods: Certain foods can exacerbate diarrhea, so it’s important to steer clear of them until your gut has fully recovered. Avoid spicy, greasy, and fatty foods, as well as dairy products. It’s best to stick to low-fiber foods until your stools become more solid.
6. Take it Easy: Allow your body enough time to rest and recuperate. Stress and fatigue can hinder the healing process, so make sure to get adequate sleep and engage in activities that help you relax, such as reading, meditating, or taking gentle walks.
7. Consult Your Doctor: If your diarrhea persists for more than a few days, or if you experience severe symptoms such as high fever, bloody stools, or dehydration, it’s important to seek medical advice. Your healthcare provider can assess your condition and provide appropriate treatment options.
Conclusion
Remember, everyone’s body is different, and recovery time may vary. While these steps can help in recovering normal intestinal function after taking antibiotics, it’s always wise to follow your doctor’s instructions and seek professional guidance if needed. Be patient and kind to your body as it works its way back to optimal health.