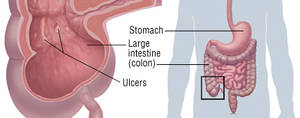
Crohn’s disease is an inflammatory bowel disease (IBD). It causes inflammation of the lining of your digestion tract, which can lead to abdominal pain, severe diarrhea, tiredness, weight-loss and malnutrition. Swelling caused by Crohn’s disease can involve different areas of the digestion tract in different individuals.
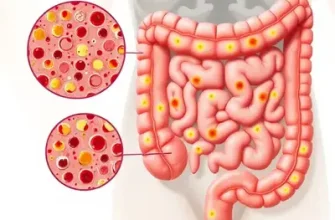
The inflammation caused by Crohn’s disease typically spreads out deep into the layers of impacted bowel tissue. Crohn’s disease can be both painful and incapacitating, and sometimes may lead to life-threatening complications.
While there’s no known remedy for Crohn’s disease, therapies can considerably minimize its signs and symptoms as well as bring about long-term remission. With treatment, many individuals with Crohn’s disease have the ability to operate well.
In some people with Crohn’s disease, only the last sector of the small intestine (ileum) is influenced. In others, the disease is confined to the colon (part of the huge intestine). The most common areas affected by Crohn’s disease are the last part of the small intestine and the colon.
Symptoms
Signs and symptoms of Crohn’s disease can vary from moderate to severe. They typically develop progressively, however sometimes will come on unexpectedly, without caution. You might likewise have time periods when you have no signs or symptoms (remission).
When the disease is active, symptoms and signs may consist of:
- Diarrhea. Diarrhea is a typical problem for people with Crohn’s disease. Heightened digestive tract cramping likewise can add to loose stools.
- Fever and fatigue. Many individuals with Crohn’s disease experience a low-grade fever, likely due to swelling or infection. You may also feel tired or have low energy.
- Abdominal pain and cramping. Inflammation and ulceration can affect the normal motion of contents through your digestive tract and may lead to pain and cramping. You might experience anything from slight discomfort to severe pain, including queasiness and throwing up.
- Blood in your stool. You may observe intense red blood in the toilet bowl or darker blood combined with your stool. You can likewise have bleeding you don’t see (occult blood).
- Mouth sores. You might have ulcers in your mouth just like canker sores.
- Minimized hunger and effective weight loss. Abdominal pain and cramping and the inflammatory response in the wall of your bowel can impact both your appetite and your capability to absorb and absorb food.
- Perianal disease. You might have pain or drain near or around the anus due to swelling from a tunnel into the skin (fistula).
Other symptoms and signs
Individuals with severe Crohn’s disease might also experience:
- Inflammation of skin, eyes and joints
- Inflammation of the liver or bile ducts
- Delayed growth or sexual development, in children
When to see a doctor
See your doctor if you have consistent changes in your bowel habits or if you have any of the symptoms and signs of Crohn’s disease, such as:
- Abdominal pain
- Blood in your stool
- Continuous bouts of diarrhea that do not react to non-prescription (OTC) medications
- Unexplained fever lasting more than a day or more
- Unusual weight reduction
Causes
The precise reason for Crohn’s disease stays unknown. Formerly, diet and stress were believed, today medical professionals know that these elements may intensify but don’t cause Crohn’s disease. A variety of aspects, such as heredity and a malfunctioning immune system, likely play a role in its development.
- Immune system. It’s possible that a virus or germs may activate Crohn’s disease. When your body immune system attempts to fight off the invading microbe, an unusual immune reaction causes the body immune system to attack the cells in the digestive tract, too.
- Genetics. Crohn’s is more common in people who have member of the family with the disease, so genes may play a role in making people more vulnerable. Nevertheless, many people with Crohn’s disease do not have a family history of the disease.
Crohn’s Disease Treatment Options and Guidelines
Treatment for Crohn’s disease usually involves drug therapy or, in specific cases, surgery. There is currently no remedy for the disease, and there is nobody treatment that works for everyone. Physicians utilize one of two approaches to treatment– either “step-up,” which begins with milder drugs first, or “top-down,” which provides people more powerful drugs earlier in the treatment process.
The goal of medical treatment is to decrease the inflammation that activates your signs and symptoms. It is likewise to enhance long-lasting diagnosis by restricting problems. In the best cases, this may lead not just to symptom relief however likewise to long-lasting remission.
Anti-inflammatory drugs
Anti-inflammatory drugs are frequently the primary step in the treatment of inflammatory bowel disease. They consist of:
- Oral 5-aminosalicylates. These drugs might be useful if Crohn’s disease influences your colon, however they aren’t practical treating disease in the small intestine. They consist of sulfasalazine (Azulfidine), which consists of sulfa, and mesalamine (Asacol, Delzicol, Pentasa, Lialda, Apriso). These drugs, particularly sulfasalazine, have a number of side effects, consisting of nausea, diarrhea, vomiting, heartburn and headache. These drugs have been commonly used in the past today are generally considered of restricted advantage.
- Corticosteroids. Corticosteroids such as prednisone can help in reducing inflammation anywhere in your body, but they have many side effects, consisting of a puffy face, excessive facial hair, night sweats, sleeping disorders and hyperactivity. More-serious side effects consist of hypertension, diabetes, osteoporosis, bone fractures, cataracts, glaucoma and increased opportunity of infection.
Likewise, corticosteroids do not work for everybody with Crohn’s disease. Medical professionals normally utilize them only if you do not react to other treatments. A more recent type of corticosteroid, budesonide (Entocort EC), works much faster than do standard steroids and appears to produce fewer side effects. Nevertheless, it is only reliable for Crohn’s disease that’s in certain parts of the bowel.
Corticosteroids aren’t for long-term usage. But they can be utilized for short-term (3 to four months) symptom improvement and to induce remission. Corticosteroids may likewise be made use of with an immune system suppressor– the corticosteroids can induce remission, while the body immune system suppressors can assist keep it.
Body immune system suppressors
These drugs also minimize inflammation, however they target your body immune system, which produces the substances that cause swelling. For some people, a combination of these drugs works better than one drug alone. Immunosuppressant drugs include:
- Azathioprine (Imuran) and mercaptopurine (Purinethol). These are the most extensively used immunosuppressants for treatment of inflammatory bowel disease. Taking them needs that you follow up closely with your doctor and have your blood inspected frequently to try to find side effects, such as a reduced resistance to infection.
Short term, they likewise can be related to inflammation of the liver or pancreas and bone marrow suppression. Long term, although hardly ever, they are connected with certain infections and cancers including lymphoma and skin cancer. They may likewise cause queasiness and vomiting. Your doctor will use a blood test to identify whether you can take these medications.
- Infliximab (Remicade), adalimumab (Humira) and certolizumab pegol (Cimzia). These drugs, called TNF inhibitors or “biologics,” work by reducing the effects of an immune system protein referred to as growth necrosis aspect (TNF). They are made use of for grownups and children with moderate to severe Crohn’s disease to reduce signs and symptoms. They likewise may induce remission. Scientists continue to study these drugs to compare their advantages.
TNF inhibitors might be used soon after medical diagnosis, especially if your doctor suspects that you’re most likely to have more severe Crohn’s disease or if you have a fistula. Often they are utilized after other drugs have actually failed. They likewise may be integrated with an immunosuppressant in some individuals, but this practice is rather controversial.
Individuals with certain conditions cannot take TNF inhibitors. Tuberculosis and other serious infections have been connected with the use of immune-suppressing drugs. Talk to your doctor about your possible threats and have a skin test for tuberculosis, a chest X-ray and a test for hepatitis B prior to beginning these medications. They are also connected with certain cancers, including lymphoma and skin cancers.
- Methotrexate (Rheumatrex). This drug, which is utilized to deal with cancer, psoriasis and rheumatoid arthritis, is sometimes made use of for individuals with Crohn’s disease who don’t respond well to other medications.
Short-term side effects consist of queasiness, fatigue and diarrhea, and rarely, it can cause possibly dangerous pneumonia. Long-term usage can lead to bone marrow suppression, scarring of the liver and in some cases to cancer. You will have to be followed carefully for side effects.
- Cyclosporine (Gengraf, Neoral, Sandimmune) and tacrolimus (Astagraf XL, Hecoria). These potent drugs, often made use of to assist recover Crohn’s-relevant fistulas, are typically booked for individuals who have not reacted well to other medications. Cyclosporine has the potential for serious side effects, such as kidney and liver damage, seizures, and deadly infections. These medications aren’t for long-term usage.
- Natalizumab (Tysabri) and vedolizumab (Entyvio). These drugs work by stopping specific immune cell molecules- integrins– from binding to other cells in your digestive tract lining. Natalizumab is authorized for people with moderate to severe Crohn’s disease with proof of inflammation who aren’t reacting well to any other medications.
Because the drug is related to an unusual however major risk of progressive multifocal leukoencephalopathy– a brain disease that usually leads to death or severe impairment– you must be registered in an unique limited distribution program to use it.
Vedolizumab recently was authorized for Crohn’s disease. It works like natalizumab however appears not to carry a risk of brain disease.
- Ustekinumab (Stelara). This drug is made use of to treat psoriasis. Researches have revealed it’s helpful in treating Crohn’s disease also and may be utilized when other medical treatments fail.
Crohn’s Disease Treatment with Antibiotics
Antibiotics can reduce the amount of drain and in some cases recover fistulas and abscesses in people with Crohn’s disease. Some researchers also believe antibiotics help reduce damaging digestive bacteria that may play a role in activating the digestive tract body immune system, resulting in inflammation.
Antibiotics may be made use of in addition to other medications or when infection is a concern, such as with perianal Crohn’s disease. However, there’s no strong proof that antibiotics are effective for Crohn’s disease. Often prescribed antibiotics consist of:
- Metronidazole (Flagyl). At one time, metronidazole was the most frequently utilized antibiotic for Crohn’s disease. However, it can cause severe side effects, consisting of numbness and tingling in your hands and feet and, periodically, muscle pain or weakness. If these results occur, stop the medication and call your doctor.
Ciprofloxacin (Cipro). This drug, which improves symptoms in some individuals with Crohn’s disease, is now generally liked to metronidazole. An unusual side effect is tendon rupture, which is an enhanced risk if you’re also taking corticosteroids.
Other medications
In addition to controlling swelling, some medications might assist eliminate your symptoms and signs, however always speak to your doctor before taking any non-prescription medications. Depending upon the intensity of your Crohn’s disease, your doctor may suggest one or more of the following:
- Anti-diarrheals. A fiber supplement, such as psyllium powder (Metamucil) or methylcellulose (Citrucel), can help alleviate mild to moderate diarrhea by adding bulk to your stool. For more severe diarrhea, loperamide (Imodium) may be effective. Anti-diarrheals must just be made use of after conversation with your doctor.
- Painkiller. For moderate pain, your doctor may recommend acetaminophen (Tylenol, others)– however not other common pain relievers, such as ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, Anaprox). These drugs are most likely making your symptoms even worse, and can make your disease even worse too.
- Iron supplements. If you have chronic digestive bleeding, you might establish iron deficiency anemia and have to take iron supplements.
- Vitamin B-12 shots. Crohn’s disease can cause Vitamin B-12 shortage. Vitamin B-12 assists avoid anemia, promotes typical growth and development, and is vital for correct nerve function.
- Calcium and vitamin D supplements. Crohn’s disease and steroids made use of to treat it can increase your risk of osteoporosis, so you may have to take a calcium supplement with included vitamin D.
Nutrition therapy
Your doctor might recommend an unique diet given via a feeding tube (enteral nutrition) or nutrients injected into a vein (parenteral nutrition) to treat your Crohn’s disease. This can enhance your general nutrition and enable the bowel to rest. Bowel rest can decrease inflammation in the short term.
Your doctor may use nutrition therapy short term and combine it with medications, such as body immune system suppressors. Enteral and parenteral nutrition are usually made use of to obtain people much healthier prior to surgery or when other medications cannot manage symptoms.
Your doctor might also suggest a low residue or low-fiber diet to reduce the risk of intestinal tract blockage if you have actually a narrowed bowel (stricture). A low residue diet is created to decrease the size and variety of your stools.
Crohn’s Disease & Surgery
If diet and way of life changes, drug therapy or other treatments don’t eliminate your symptoms and signs, your doctor might suggest surgery. As much as one-half of people with Crohn’s disease will need at least one surgery. Nevertheless, surgery does not cure Crohn’s disease.
During surgery, your specialist eliminates a damaged portion of your digestion tract and then reconnects the healthy sections. Surgery might also be made use of to close fistulas and drain abscesses. A typical procedure for Crohn’s disease is strictureplasty, which expands a section of the intestinal tract that has become too slim.
The advantages of surgery for Crohn’s disease are typically temporary. The disease often repeats, often near the reconnected tissue. The best strategy is to follow surgery with medication to minimize the risk of recurrence.