If you’ve recently been diagnosed with a fibroadenoma, you might be wondering whether it needs to be removed.
What Exactly Is a Fibroadenoma?
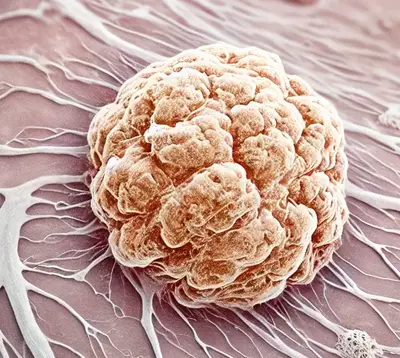
A fibroadenoma is a non-cancerous breast lump that often feels firm, smooth, and moveable under the skin. It’s the most common type of benign breast tumor, especially in women between the ages of 15 and 35. These lumps are made up of glandular and connective tissue and are typically painless. Statistically, fibroadenomas occur in about 10% of women at some point in their lives (source).
Do All Fibroadenomas Require Removal?
Fibroadenoma Size and Decision to Remove (Europe & USA)
| Size of Fibroadenoma | Frequency of Removal (%) |
|---|---|
| Up to 2 cm (0.8 in) | 20% |
| 2-4 cm (0.8-1.6 in) | 35% |
| 4-6 cm (1.6-2.4 in) | 50% |
| More than 6 cm (2.4 in) | 70% |
This histogram illustrates the frequency of fibroadenoma removal by size, represented in both centimeters (Europe) and inches (USA). Larger fibroadenomas are more likely to be surgically removed.
The short answer is no, not all fibroadenomas need to be removed. Most fibroadenomas are harmless and do not increase your risk of breast cancer. They are often left alone and simply monitored for changes. In fact, the standard approach for fibroadenomas is ‘watchful waiting’—meaning your doctor will monitor the lump for any changes in size or characteristics.
Frequency of Fibroadenoma Removal by Age Group
| Age Group | Frequency of Removal (%) |
|---|---|
| 20-30 | 40% |
| 30-40 | 30% |
| 40-50 | 20% |
| 50+ | 10% |
This histogram illustrates the frequency of fibroadenoma removal in different age groups. Younger women are more likely to opt for removal compared to older age groups.
Did You Know?
Only about 10% of fibroadenomas grow in size, and even fewer become symptomatic or problematic (source). Most women can live with fibroadenomas without any issues.
When Should a Fibroadenoma Be Removed?
There are specific situations in which removing a fibroadenoma may be recommended:
- Size Increase: If the fibroadenoma is growing or changing in size or shape, your doctor may recommend removal to rule out other conditions.
- Discomfort: Some fibroadenomas, especially larger ones, may cause discomfort or distortion of the breast. In these cases, removal may improve quality of life.
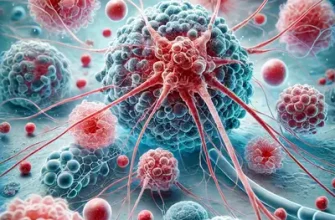
- Complex Fibroadenomas: Occasionally, fibroadenomas can have features that suggest a more complex structure. Complex fibroadenomas may have slightly increased risks associated, prompting some doctors to recommend removal.
- Patient Preference: Some patients prefer to have the fibroadenoma removed for peace of mind, especially if they are anxious about the possibility of it changing over time.
Table: Types of Fibroadenomas and Management Approaches
| Type | Characteristics | Typical Management |
|---|---|---|
| Simple Fibroadenoma | Smooth, firm, painless, stable size | Watchful waiting |
| Complex Fibroadenoma | Multiple components, increased growth risk | Often recommended removal |
| Giant Fibroadenoma | Larger than 5 cm, causes discomfort | Surgical removal |
| Juvenile Fibroadenoma | Found in younger women, rapid growth | Usually removed |
Frequency of Fibroadenoma Removal by Type
| Fibroadenoma Type | Frequency of Removal (%) |
|---|---|
| Simple Fibroadenoma | 25% |
| Complex Fibroadenoma | 40% |
| Giant Fibroadenoma | 60% |
| Juvenile Fibroadenoma | 50% |
This histogram illustrates the frequency of removal for different types of fibroadenomas. Giant and juvenile fibroadenomas are more frequently removed compared to simple fibroadenomas.
How Are Fibroadenomas Diagnosed and Treated?
Most fibroadenomas are discovered during routine breast exams or imaging studies like ultrasound or mammograms. If your doctor is unsure of the nature of the lump, a core needle biopsy may be performed. This is a minimally invasive procedure where a small sample of tissue is taken to confirm the diagnosis.
Treatment typically depends on the size, growth, and patient comfort. Surgical removal, known as a lumpectomy or excisional biopsy, is a common method for removing larger or problematic fibroadenomas. It’s a relatively simple outpatient procedure that typically costs between $2,000 to $5,000 in the U.S., depending on the facility and region.
Did You Know?
A core needle biopsy is considered the gold standard for diagnosing breast lumps, with accuracy rates of over 98% (source). This high accuracy helps doctors decide the best course of action without needing to rush to surgery.
What Are the Risks of Not Removing a Fibroadenoma?
For most women, the risks of not removing a fibroadenoma are minimal. However, in rare cases, a fibroadenoma can grow significantly, leading to breast asymmetry or discomfort. Complex fibroadenomas, while still benign, may have a slightly increased risk of developing into breast cancer compared to simple fibroadenomas, but this risk is still very low.
How Common Is Recurrence After Removal?
If a fibroadenoma is removed, there is a small chance of recurrence—about 15-20%. Sometimes, new fibroadenomas may also form. This is more common in younger women, as hormonal fluctuations during the reproductive years can influence the formation of fibroadenomas.
Did You Know?
Research indicates that fibroadenomas are hormone-sensitive and tend to shrink after menopause, when hormone levels drop (source). This is why doctors often recommend watchful waiting for older women, as the fibroadenoma may naturally regress over time.
Should You Be Worried?
If you’ve been diagnosed with a fibroadenoma, it’s important to stay informed but not overly worried. Fibroadenomas are benign and do not usually require aggressive treatment. Monitoring through regular ultrasound or mammography is often sufficient to ensure there are no changes. If changes are noted, it’s always possible to discuss removal with your healthcare provider.
Our Editorial Advice
For those diagnosed with a fibroadenoma, understanding your options is key. Always discuss your preferences and concerns with your healthcare provider, and weigh the pros and cons of removal versus monitoring. There’s no one-size-fits-all answer, and your comfort and peace of mind are important factors in making the right decision for your health.