A duodenal ulcer is usually triggered by an infection with a bacterium (bacterium) called Helicobacter pylori (H. pylori). A 4- to 8-week course of acid-suppressing medication will enable the ulcer to heal. In addition, a one-week course of 2 antibiotics plus an acid-suppressing medicine will usually clear the H. pylori infection. This usually avoids the ulcer from returning. Anti-inflammatory medications used to deal with conditions such as arthritis sometimes cause duodenal ulcers. If you have to continue with the anti-inflammatory medication then you might have to take long-lasting acid-suppressing medication.
What Is a Duodenal Ulcers?
Duodenal and gastric ulcers are typically called peptic ulcers. A peptic ulcer is an ulcer triggered by stomach acid. An ulcer happens where the lining of the gut is damaged and the underlying tissue is exposed. If you could see inside your gut, an ulcer appears like a little, red crater on the within lining of the gut.
A duodenal ulcer is an ulcer that takes place in the lining in the part of the small intestine just beyond the stomach (the duodenum). An ulcer in the lining of the stomach is called a gastric ulcer.
There are different brochures called Non-ulcer Dyspepsia (Functional Dyspepsia), Stomach Ulcer (Gastric Ulcer) and Acid Reflux and Oesophagitis.
What Causes Duodenal Ulcers?
Your stomach generally produces acid to assist with the digestion of food and to kill bacteria (germs). This acid is destructive so some cells on the inside lining of the stomach and the first part of the little intestinal tract (the duodenum) produce a natural mucous barrier. This protects the lining of the stomach and duodenum.
There is normally a balance between the amount of acid that you make and the mucous defence barrier. An ulcer might establish if there is a change in this balance, enabling the acid to damage the lining of the stomach or duodenum. Causes of this include the following:
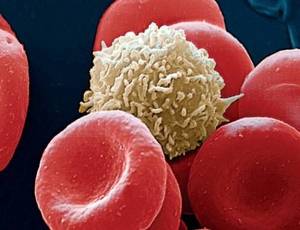
1. Infection with Helicobacter pylori (H. pylori)
Infection with H. pylori is the cause in about 19 in 20 cases of duodenal ulcer. More than a quarter of individuals in the UK become infected with H. pylori at some stage in their lives. See the different leaflet called Stomach Pain (Helicobacter Pylori) for more details.
2. Anti-inflammatory Medicines
Anti-inflammatory medications are in some cases called non-steroidal anti inflammatory drugs (NSAIDs). There are numerous types and brands. For example, aspirin, ibuprofen, diclofenac, and so on. These medications sometimes impact the mucous barrier of the duodenum and permit acid to trigger an ulcer. About 1 in 20 duodenal ulcers are triggered by anti-inflammatory medications.
3. Other Causes and Factors
Other causes are uncommon. For example, the Zollinger-Ellison syndrome. In this rare condition, far more acid than typical is made by the stomach.
Other elements such as smoking cigarettes, stress and drinking heavily might perhaps increase the threat of having a duodenal ulcer. Nevertheless, these are not typically the underlying reason for duodenal ulcers.
What Are the Symptoms of a Duodenal Ulcers?
- Pain in the upper tummy (abdomen) simply below the breastbone (breast bone) is the typical symptom. It usually comes and goes. It may occur most before meals, or when you are starving. It might be eased if you eat food, or take antacid tablets. The pain might wake you from sleep.
- Other symptoms which might occur include bloating, retching, and sensation ill. You may feel especially complete after a meal. Often food makes the pain worse.
- Issues happen in many cases and can be serious. These include:
- Bleeding ulcer. This can vary from a drip to a dangerous bleed.
- Perforation. The ulcer goes right through (bores) the wall of the first part of the little intestine (duodenum).
- Food and acid in the duodenum then leak into the stomach cavity. This usually causes extreme pain and is a medical emergency situation.
Diagnosis for Duodenal Ulcers
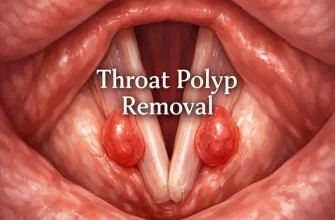
Gastroscopy (endoscopy) is the test that can confirm a duodenal ulcer. In this test a medical professional or nurse looks inside your stomach and the first part of your little intestine (duodenum). They do this by passing a thin, flexible telescope down your gullet (oesophagus). They can see any inflammation or ulcers.
A test to discover the H. pylori bacterium (germs) is normally done if you have a duodenal ulcer. If H. pylori is found then it is likely to be the cause of the ulcer. Quickly, it can be spotted in a sample of stool (faeces), or in a breath test, or from a blood test, or from a biopsy sample taken during an endoscopy.
What Are the Treatments for a Duodenal Ulcer?
General Advice
Lifestyle measures can enhance symptoms, such as:
- Lose weight if you are obese.
- Prevent any trigger foods, such as coffee, chocolate, tomatoes, fatty foods or spicy foods.
- Eat smaller sized meals and eat your evening meal 3-4 hours prior to going to bed.
- Stop smoking and alcohol drinking.
Acid-suppressing Medication
A 4- to 8-week course of a medicine that greatly minimizes the quantity of acid your stomach makes is typically advised. The most commonly used medication is a proton pump inhibitor (PPI). See the different brochure called Indigestion Medication for additional information.
If Your Ulcer Was Caused by H. Pylori
Nearly all duodenal ulcers are brought on by infection with H. pylori. Therefore, a main part of the treatment is to clear this infection. If this infection is unclear, the ulcer is most likely to return once you stop taking acid-suppressing medication. See the different leaflet called Stomach Pain (Helicobacter Pylori) for additional information.
If Your Ulcer Was Caused by an Anti-inflammatory Medicine
If possible, you should stop the anti-inflammatory medicine. This permits the ulcer to heal. You will likewise usually be recommended an acid-suppressing medication for several weeks (as discussed above). This stops the stomach from making acid and allows the ulcer to recover.
Nevertheless, oftentimes the anti-inflammatory medication is needed to alleviate symptoms of arthritis or other unpleasant conditions, or aspirin is had to protect against embolism. In these scenarios, one choice is to take an acid-suppressing medicine every day indefinitely. This minimizes the quantity of acid made by the stomach, and greatly minimizes the opportunity of an ulcer forming once again.
Duodenal Ulcer and Surgery
In the past, surgery was typically needed to treat a duodenal ulcer. This was prior to it was discovered that H. pylori was the reason for the majority of duodenal ulcers, and before modern acid-suppressing medications became available. Surgery is now typically only needed if a complication of a duodenal ulcer develops such as severe bleeding or a hole (perforation).
Duodenal Ulcers Diet
Physicians frequently advise lifestyle and dietary changes for persons with ulcers in addition to medications till complete healing happens. Although in the previous patients were encouraged to follow a bland diet, existing research does not support this dietary adjustment to be helpful. Although hot foods are an irritant for some people with ulcers, medical professionals now position more focus on a high fibre diet rich in vegetables and fruits.
1. Dietary Fibre & Vitamin A
Research reveals that a high fiber diet decreases the danger of establishing ulcer disease. Although both insoluble and soluble fibers demonstrate this association, there is a more powerful association in between diets high in soluble fiber and a reduced danger for developing ulcers.
Foods that are high in soluble fiber include oats, psyllium husk, vegetables, flax seeds, barley, nuts, and specific vegetables and fruits, such as oranges, apples, and carrots.
Findings from a prospective mate study that included 47,806 men, showed that a diet rich in vitamin A from all sources might reduce the development of duodenal ulcer, as may diets high in vegetables and fruits, possibly due to their fibre material. A potential associate study follows, gradually, a group of similar people (accomplice) who vary with respect to particular factors under study, to figure out how these elements impact rates of a certain outcome; however, more research is necessary to confirm outcomes since there are numerous other aspects involved with this type of study that might puzzle the data.
Animal studies demonstrate that vitamin A increases the production of mucus in the intestinal tract. Impaired mucosal defense can allow ulcers to establish. For that reason, vitamin A might have a protective result versus the advancement of ulcer disease.
Great sources of vitamin An include liver, carrots, broccoli, sweet potatoes, kale, spinach, and collard greens.
2. Green Tea and Flavonoid-Rich Foods
Emerging research from China shows the potential protective impacts of green tea and other foods that are abundant in flavonoids versus chronic gastritis, H. pylori infection, and stomach cancer. Particularly, these foods seem to prevent the growth of H. pylori.
In addition, one recent lab study of green, white, oolong, and black teas indicated that these teas prevent the growth of H. pylori but trigger no harm to beneficial kinds of germs typically found in the stomach, consisting of L. acidophilus, L. plantarum, and B. lungum. Nevertheless, this was an in vitro study, which means screening took place directly between teas and bacteria in the laboratory, and we can not draw direct conclusions as to what would happen inside the body between these 2 substances. Beneficial impacts in the laboratory were best when tea steeped for a complete five minutes.
Flavonoid-rich foods include garlic, onions, and vibrant vegetables and fruits such as cranberries, strawberries, blueberries, broccoli, carrots, and snap peas.
3. Coffee and Alcohol
Both caffeinated and decaffeinated coffee can increase acid production and intensify symptoms in individuals with ulcer disease. Alcohols can deteriorate the protective mucosal lining along the gastrointestinal tract and result in more swelling and bleeding. To minimize symptoms, people with ulcer disease need to avoid or restrict coffee and give up alcohol (as iytmed.com mentioned earlier).
4. Check Your Individual Tolerance
No proof recommends that spicy or citrus foods affect ulcer disease, although some individuals do report aggravating of symptoms after consuming these types of foods. It is important to learn what works for you. If you discover that your symptoms become worse after eating particular foods, then limit or prevent them so you can feel your best, making sure that you do not remove a whole food group.