High carbon dioxide in blood means the body is holding on to more CO₂ than it should, often because the lungs can’t clear it efficiently. It’s similar to a room with poor ventilation — the air becomes heavy, and everything starts to feel harder. This understanding helps frame why even mild changes in breathing can matter.
High carbon dioxide that gradually builds up in the blood often appears in chronic lung conditions, affecting millions of adults in the U.S. each year. It’s more common in people with longstanding respiratory issues, reduced lung capacity, or certain neurological conditions that slow breathing patterns. The risk increases with age, limited physical activity, and untreated airway inflammation.
After an episode of shortness of breath or unusual fatigue, when someone notices repeat sensations of heaviness or dull headaches that follow, a rising level of carbon dioxide can be part of the explanation. Recognizing how this imbalance develops makes it easier to understand the symptoms and the steps used to correct them.
Common Symptoms of Hypercapnia
This chart illustrates the prevalence of common symptoms of hypercapnia, with headache and shortness of breath being the most frequently reported.
Causes of Elevated CO2 Levels
- Chronic Obstructive Pulmonary Disease (COPD): A leading cause of CO2 retention due to impaired lung function and inadequate gas exchange. Patients with COPD often experience chronic shortness of breath, wheezing, and a persistent cough. As lung function declines, CO2 levels rise, leading to increased fatigue, confusion, and, in severe cases, respiratory failure.
- Sleep Apnea: Repeated breathing interruptions during sleep can lead to CO2 buildup in the bloodstream. Individuals with untreated sleep apnea may wake up frequently at night gasping for air and feel excessively drowsy during the day. Prolonged CO2 retention can contribute to cognitive impairment, cardiovascular issues, and even increase the risk of stroke.
- Obesity Hypoventilation Syndrome (OHS): Excess weight can restrict lung expansion, reducing effective CO2 elimination. Patients with OHS often struggle with chronic fatigue, morning headaches, and breathlessness, especially when lying down. In extreme cases, CO2 buildup can lead to respiratory failure, necessitating ventilatory support.
- Lung Diseases (e.g., Asthma, Pulmonary Fibrosis): Poor oxygen exchange results in CO2 retention. Asthma attacks can cause CO2 levels to spike due to airway constriction, leading to panic, confusion, and an inability to speak. Pulmonary fibrosis, which scars lung tissue, progressively reduces gas exchange efficiency, causing chronic hypercapnia.
- Neuromuscular Disorders (e.g., ALS, Myasthenia Gravis): Weak respiratory muscles reduce breathing efficiency, leading to CO2 accumulation. Patients with ALS may experience progressive weakness in their breathing muscles, making it difficult to expel CO2. In later stages, non-invasive ventilation or mechanical ventilation may be required to sustain life.
- Sedative or Opioid Overdose: These drugs depress the respiratory system, causing hypoventilation and CO2 retention. Overdose cases often present with slowed breathing, pinpoint pupils, and unconsciousness. If untreated, high CO2 levels can lead to coma or death, requiring emergency naloxone administration and ventilatory support.
- Kidney Dysfunction: The kidneys regulate acid-base balance; failure to excrete excess CO2 can result in hypercapnia. Chronic kidney disease patients may experience acid buildup in the blood (acidosis), exacerbating CO2 retention and leading to symptoms such as confusion, rapid breathing, and muscle twitching.
Annual Costs of Managing Chronic Hypercapnia (USD per Year)
| Expense Category | Cost (USD) |
|---|---|
| CPAP/BiPAP Machine & Supplies | $1,200 |
| Oxygen Therapy | $1,500 |
| Medications (Bronchodilators, Diuretics) | $800 |
| Pulmonary Rehab Sessions | $2,000 |
| Regular Doctor Visits & Tests | $1,000 |
This chart outlines the annual costs associated with managing chronic hypercapnia, highlighting the financial burden of essential treatments and therapies.
Symptoms of High CO2 Levels
Mild to moderate hypercapnia may present with symptoms such as:
- Headache: Unlike a tension headache, CO2-related headaches often come with dizziness and a feeling of mental fog. They tend to worsen when lying down or in enclosed spaces.
- Dizziness: This is more of a lightheaded sensation rather than vertigo. It often occurs alongside confusion and shortness of breath, differentiating it from dehydration or simple exhaustion.
- Shortness of breath: Unlike exertional breathlessness, CO2-related dyspnea can feel suffocating even at rest. It may worsen when lying down and improve slightly with upright positioning.
- Confusion: This symptom sets hypercapnia apart from other respiratory conditions. It often appears as delayed responses, trouble concentrating, or an odd sense of detachment.
- Flushed skin: Unlike fever-related flushing, CO2-induced flushing presents with warm, red skin, especially on the face, often without a rise in body temperature.
Severe cases can lead to:
- Disorientation: Unlike typical confusion, this progresses rapidly and may involve difficulty recognizing familiar people or surroundings.
- Muscle twitching: A sign of CO2 affecting neuromuscular function, it appears as small, involuntary muscle contractions, often in the hands or face.
- Increased heart rate: The heart beats faster in an attempt to compensate for the respiratory inefficiency, often accompanied by palpitations and anxiety.
- Unconsciousness: If CO2 levels rise too high, oxygen deprivation can lead to loss of consciousness, differing from fainting in that it does not respond quickly to position changes.
- Respiratory failure: The most dangerous stage, where breathing slows dangerously or stops altogether, requiring immediate intervention such as mechanical ventilation.
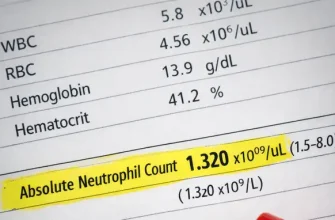
Diagnosis of Hypercapnia
Diagnostic methods include:
- Arterial Blood Gas (ABG) Test: Measures CO2, oxygen, and pH levels in the blood. The test involves drawing blood from an artery, typically the wrist, which can cause moderate discomfort due to the artery’s sensitivity. Patients may feel a sharp pinch and mild soreness afterward. (Accuracy: 9/10; Cost: $100–$300)
- Pulmonary Function Tests: Assess lung capacity and airflow. The patient is required to breathe forcefully into a mouthpiece connected to a machine, which can cause mild dizziness or breathlessness in some individuals. (Accuracy: 8/10; Cost: $150–$350)
- Capnography: Monitors exhaled CO2 levels in real-time. A small sensor is placed near the nostrils or inside an oxygen mask. It is non-invasive and painless, though some patients might find the sensation of airflow monitoring mildly uncomfortable. (Accuracy: 7/10; Cost: $200–$500)
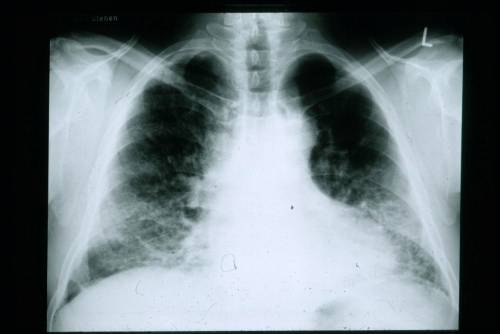
- Chest X-ray or CT Scan: Identifies lung abnormalities contributing to CO2 retention. The procedure is quick and painless, though some patients may feel anxious about remaining still during imaging. A CT scan may require contrast dye injection, which can cause a warm sensation. (Accuracy: 7/10; Cost: $150–$1,000)
Severity Levels of Hypercapnia (PaCO2 mmHg)
| Severity Level | Prevalence (%) |
|---|---|
| Mild (45-55 mmHg) | 40% |
| Moderate (56-70 mmHg) | 35% |
| Severe (>70 mmHg) | 25% |
This chart categorizes hypercapnia severity levels based on PaCO2 measurements, illustrating their prevalence among affected individuals.
Real Medical Cases
- Case 1: A 68-year-old male from New York with COPD experienced worsening shortness of breath. ABG tests revealed CO2 retention, requiring BiPAP therapy, which improved his condition.
- Case 2: A 45-year-old woman from Texas overdosed on opioids, leading to respiratory depression. She was placed on mechanical ventilation until her CO2 levels normalized.
Risk Factors for Developing Hypercapnia
This chart highlights key risk factors for developing hypercapnia, with smoking and chronic lung disease being the most significant contributors.
Editorial Advice
Reyus Mammadli, healthcare advisor, emphasizes the importance of early detection and intervention for hypercapnia. “Managing underlying conditions like COPD and sleep apnea significantly reduces the risk of CO2 buildup. Regular medical checkups, lifestyle changes, and adherence to prescribed treatments are key to maintaining balanced CO2 levels.”
For individuals at risk, investing in a home pulse oximeter and seeking immediate medical attention for persistent symptoms can prevent severe complications.
Most Affected Age Groups
| Age Group | Prevalence (%) |
|---|---|
| 0-18 years | 10% |
| 19-40 years | 20% |
| 41-60 years | 40% |
| 61+ years | 60% |
This chart shows the age groups most affected by hypercapnia, with older individuals being at the highest risk.
References
- American Lung Association – Information on COPD, lung diseases, and respiratory failure. https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd/treating
- National Institutes of Health (NIH) – Research on hypercapnia, symptoms, and diagnosis methods. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7117473/
- Mayo Clinic – Data on sleep apnea, obesity hypoventilation syndrome, and related complications. https://www.mayoclinic.org/diseases-conditions/sleep-apnea/symptoms-causes/syc-20377631
- Centers for Disease Control and Prevention (CDC) – Guidelines on opioid overdose and respiratory depression. https://www.cdc.gov/drugoverdose/index.html
- American Thoracic Society – Insights into pulmonary function tests and BiPAP therapy. https://www.thoracic.org/professionals/clinical-resources/pulmonary-function-testing/
- New England Journal of Medicine – Clinical studies on CO2 retention and treatment options. https://www.nejm.org/doi/full/10.1056/NEJMra2023674
- World Health Organization (WHO) – Global perspectives on respiratory diseases and non-invasive ventilation. https://www.who.int/news-room/fact-sheets/detail/noninvasive-ventilation