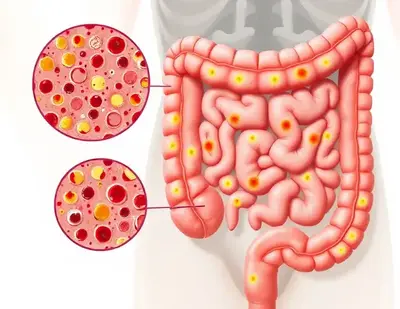
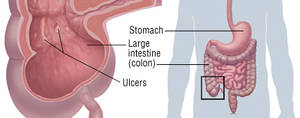
Inflammatory Bowel Disease (IBD) is a chronic condition that causes inflammation of the digestive tract. The two main types of IBD are Crohn’s disease and ulcerative colitis. While Crohn’s can affect any part of the gastrointestinal (GI) tract, ulcerative colitis is limited to the colon and rectum. IBD impacts millions worldwide, with the U.S. alone having over 3 million diagnosed cases.
Global Prevalence of Inflammatory Bowel Disease (IBD) by Region (2024)
This chart visualizes the prevalence of Inflammatory Bowel Disease (IBD) across different global regions in 2024. North America has the highest number of cases, while Africa has the lowest.
Common Symptoms of IBD
IBD symptoms vary depending on severity and location but often include:
- Abdominal pain and cramping – Common in both Crohn’s disease and ulcerative colitis. Patients often describe the pain as a deep, persistent ache that worsens after meals and sometimes wakes them at night.
- Diarrhea – Can be severe and persistent, sometimes containing mucus or blood. Patients often experience urgency, which can significantly impact their daily routines and social lives.
- Bloody stool – More frequent in ulcerative colitis. Seeing blood in stool can be alarming, and persistent bleeding may lead to anemia, causing dizziness and weakness.
- Weight loss – Due to malabsorption and reduced appetite. Some individuals struggle to maintain weight despite a high-calorie diet.
- Fatigue – Often caused by chronic inflammation. Many patients report feeling constantly drained, making it difficult to work or engage in normal activities.
- Fever – A sign of active inflammation. Fevers can appear suddenly and may be accompanied by chills and night sweats.
How Dangerous Is IBD?
IBD can be particularly dangerous when combined with other conditions. For instance, patients who also suffer from anemia due to chronic blood loss may develop severe fatigue and heart palpitations. Persistent inflammation increases the risk of colon cancer, particularly in those with long-standing ulcerative colitis. Additionally, uncontrolled IBD can lead to toxic megacolon, a life-threatening complication where the colon rapidly expands, causing severe pain and risk of rupture.
Causes and Risk Factors
Though the exact cause remains unknown, IBD is believed to result from an abnormal immune response. Key risk factors include:
- Genetics – A family history increases the risk. Many patients report multiple family members with similar digestive disorders.
- Immune system dysfunction – The immune system mistakenly attacks gut tissues, leading to chronic inflammation.
- Environmental factors – Diet, smoking, and stress can trigger flare-ups. Many patients report worsening symptoms after consuming processed foods or undergoing stressful life events.
- Age and ethnicity – Most cases develop before age 30, and some ethnic groups, such as Ashkenazi Jews, have a higher prevalence.
Common Triggers for IBD Flare-Ups (Patient-Reported, % of Cases)
| Trigger | % of Cases |
|---|---|
| Stress | 60% |
| Diet (spicy, processed foods) | 50% |
| Lack of Sleep | 45% |
| Infection | 40% |
| Medication Non-Adherence | 35% |
This chart highlights the most common patient-reported triggers for IBD flare-ups, with stress being the most frequently cited factor.
Diagnosis: How Is IBD Identified?
A proper diagnosis requires multiple tests and imaging techniques. Some of the most effective diagnostic tools include:
- Colonoscopy and Biopsy – Directly examines the colon lining and collects tissue samples (Accuracy: 90% | Cost: $2,000–$3,500). Patients may experience mild discomfort and bloating after the procedure. It is one of the most commonly used diagnostic methods due to its high accuracy and ability to detect early signs of IBD. Many describe the preparation process, involving strong laxatives, as the most challenging part.
- MRI and CT Scans – Provides detailed images of the GI tract (Accuracy: 85% | Cost: $1,500–$3,000). Patients typically experience no pain but may need to ingest a contrast dye, which can cause mild nausea. These scans are widely used for evaluating disease extent and complications, especially when strictures or fistulas are suspected.
- Stool Tests – Detects inflammation markers like calprotectin (Accuracy: 75% | Cost: $200–$500). This non-invasive test is simple but may be inconvenient for some patients. It is growing in popularity due to its ease of use and ability to monitor disease activity. Patients often feel relieved when this test provides insights without requiring invasive procedures.
- Blood Tests – Measures inflammatory markers like C-reactive protein (Accuracy: 70% | Cost: $50–$200). This is a routine, low-cost test but lacks specificity, meaning additional tests are usually required. Patients with frequent flares may require ongoing blood work to monitor inflammation levels.
IBD-Related Hospitalization Rates by Age Group (2024, per 100,000 people)
| Age Group | Hospitalization Rate |
|---|---|
| 0-17 years | 25 |
| 18-34 years | 80 |
| 35-49 years | 110 |
| 50-64 years | 150 |
| 65+ years | 200 |
This chart presents hospitalization rates for IBD across different age groups in 2024, with the highest rates among individuals aged 65 and older.
Modern Treatment Options
Treatment for IBD has advanced significantly, with new medications and procedures improving patient outcomes. The primary treatment options include:
1. Medications
- Biologics (e.g., Infliximab, Adalimumab) – Target specific immune pathways to reduce inflammation. Many patients experience significant improvement, although some report side effects like increased susceptibility to infections.
- Immunosuppressants (e.g., Azathioprine, Methotrexate) – Help prevent immune system overactivity by suppressing abnormal immune responses. These medications are often used alongside biologics for greater effectiveness.
- Anti-Inflammatory Drugs (e.g., Mesalamine, Sulfasalazine) – Reduce symptoms in mild to moderate cases by decreasing inflammation in the intestinal lining. Long-term use may help prevent flare-ups.
- Corticosteroids (e.g., Prednisone) – Short-term use for severe flare-ups. While effective, prolonged use can lead to significant side effects such as osteoporosis and adrenal suppression, making them a last-resort option.
- JAK Inhibitors (e.g., Tofacitinib) – A newer class of drugs targeting specific inflammation pathways in the immune system, offering hope for patients with moderate to severe IBD who do not respond to other treatments.
Cost of IBD Treatment Options (Annual Average per Patient in USD)
| Treatment Option | Annual Cost (USD) |
|---|---|
| Biologics | $25,000 |
| Immunosuppressants | $12,000 |
| Anti-Inflammatory Drugs | $8,000 |
| Surgery | $50,000 |
| Probiotic & Dietary Therapy | $3,500 |
This chart presents the annual average cost of various IBD treatment options, highlighting surgery as the most expensive option.
Medical Case: Real-World Example
A 32-year-old woman from Chicago suffered from chronic diarrhea and severe abdominal pain for five years. After multiple misdiagnoses, a colonoscopy confirmed ulcerative colitis. She began biologic therapy (Adalimumab), which reduced her symptoms by 80% within six months. Today, she maintains remission with lifestyle adjustments and periodic medication. Additionally, she follows a low-FODMAP diet and undergoes routine monitoring to prevent complications, allowing her to lead an active and fulfilling life. She describes her journey as “a battle, but one that I now feel equipped to handle.”
Percentage of IBD Patients in Remission by Treatment Type (2024)
This chart presents the percentage of IBD patients in remission by treatment type in 2024, with surgery showing the highest remission rate.
Editorial Advice
Reyus Mammadli, healthcare advisor, emphasizes the importance of early detection and personalized treatment. Since IBD symptoms can mimic other conditions, seeking medical attention early can prevent severe complications. Patients should also work closely with a gastroenterologist to identify the most effective treatment plan.
With the rapid development of biologic therapies and precision medicine, the future for IBD patients looks promising. Staying informed and proactive can significantly improve quality of life. Newer therapies like JAK inhibitors and targeted biologics offer additional hope for those who struggle with traditional treatments.