Median arcuate ligament syndrome (MALS) is a condition in which the median arcuate ligament presses too securely on the celiac artery (a major branch of the aorta that provides blood to the stomach, liver, and other organs) and the nerves in the area (celiac plexus).
What Is Median Arcuate Ligament Syndrome?
Median arcuate ligament syndrome (MALS) is a condition in which the median arcuate ligament presses too firmly on the celiac artery (a significant branch of the aorta that provides blood to the stomach, liver, and other organs) and the nerves in the area (celiac plexus).
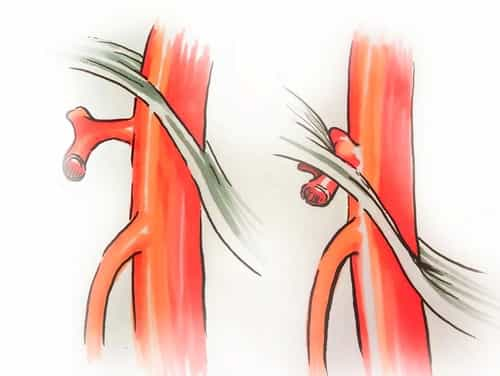
Ligaments are bands of tissue that connect one bone or cartilage to another. The median arcuate ligament is shaped like an arch and goes around the aorta (the artery in the heart that brings blood throughout the body) to connect the diaphragm to the spine.
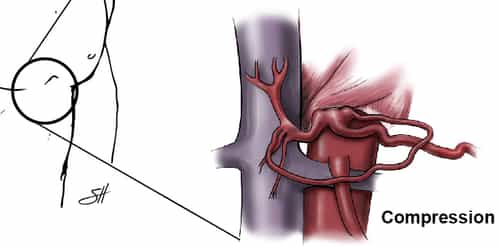
In a client with MALS, the median arcuate ligament acts like a hammer, and the celiac axis imitates an anvil, compressing (squeezing) the nerves in between. This causes a variety of symptoms, such as pain in the abdominal area that can be made worse by consuming or activity.
It is essential to differentiate median arcuate ligament syndrome (MALS) from median arcuate ligament compression. Median arcuate ligament compression occurs in about 10-25% of the population and does not trigger any symptoms. In a minimal number of these individuals, MALS exists, and patients will have the symptoms noted below.
MALS frequently occurs in thin, younger women. It is a rare condition.
Symptoms of Median Arcuate Ligament Syndrome
The first sign of MALS is a pain in the upper abdominal area after consuming. The pain triggers patients to prevent consuming, which can lead to weight loss (typically more than 20 pounds). Other associated symptoms may consist of:
- Nausea
- Diarrhea
- Throwing up
- Delayed gastric emptying (a hold-up in food moving from the stomach into the little intestinal tract).
What Causes Median Arcuate Ligament Syndrome?
It is thought that MALS is caused by the median arcuate ligament compressing or pinching the celiac plexus nerves over the celiac artery. The squeezing of these nerves can cause a pain similar to the pain patients with carpal tunnel syndrome to feel in their hands. Another cause may be the lack of blood flow to the organs provided by the celiac artery, though this theory is controversial.
How Is Median Arcuate Ligament Syndrome Diagnosed?
If your doctor believes you might have MALS, she or he will review your medical history and perform a physical examination. The medical professional may likewise buy specific tests, including blood work and imaging tests, to help eliminate more typical causes of your symptoms, such as gastroesophageal reflux disease (GERD), gastritis, gastroparesis, or issues with your pancreas, liver, gallbladder, spleen, or intestines.
Once these conditions are eliminated, your doctor may purchase a test called a mesenteric duplex ultrasound to check blood circulation through the celiac artery and compression of the celiac plexus. Another handy imaging test would be a CT or MRI angiogram, which can provide a much better image of your celiac artery and aorta.
Once the diagnosis of MALS is thought, our procedure at the Cleveland Clinic consists of a three-step procedure:
- Your records will be examined, and any additional imaging tests will be duplicated or bought (such as a mesenteric ultrasound of the celiac axis or a CT/MRI angiogram).
- You will be examined by among our minimally invasive surgery specialists in the Section of Surgical Endoscopy of the Digestive Disease and Surgery Institute. A vascular cosmetic surgeon in the Heart and Vascular Surgery Institute will likewise be readily available for consultation in more intricate cases if needed.
- You will likewise be evaluated by one of our pain management professionals for a possible celiac plexus block treatment. This offers momentary relief from the symptoms of MALS and helps to confirm the diagnosis for the patient and the entire medical group.
What Is a Celiac Plexus Block?
A celiac plexus block is an injection of medication to help alleviate pain in the abdominal area.
If you have a celiac plexus block, you will be given an intravenous medication to relax you. Then you will rest on your stomach on an x-ray table. The medical professional will numb an area of skin on your back with a local anesthetic. Then, guided by an x-ray, the physician will:
- Place a thin needle into your back, beside your spine, and inject an anesthetic.
- Insert a 2nd needle on the other side of your spine.
- Inject dye to make sure the medication goes to the correct spot.
- Inject pain medication, such as epinephrine, clonidine, or asteroid. Alcohol or phenol likewise may be injected to ruin the nerves.
The procedure usually takes less than 30 minutes, and you can go home the very same day. Your abdominal area might feel warm, and you may start to feel less abdominal pain.
Patients usually need a series of injections (between 2 and 10) to continue the pain relief. For some individuals, a celiac plexus block can eliminate pain for weeks. For others, the relief can last years. Many can go back to their normal activities.
MALS Treatment
Once the medical diagnosis of MALS is confirmed, most patients will be offered a minimally invasive (laparoscopic/robotic) technique to easing the compression of the median arcuate ligament on the aorta. In this strategy, the surgeon makes 5 to 6 little (approximately 1/2 inch) incisions (cuts) and inserts instruments to separate the median arcuate ligament and divide the nerves (neurolysis).
Most patients who have laparoscopic surgery for MALS stay overnight in the health center and begin eating a regular diet the next early morning. Patients will have some discomfort and pain from the incisions and will receive medications to relieve the pain. Many patients state that their MALS symptoms, such as pain with consuming, improve after the surgery. Most patients can return to normal activities within two to 4 weeks.
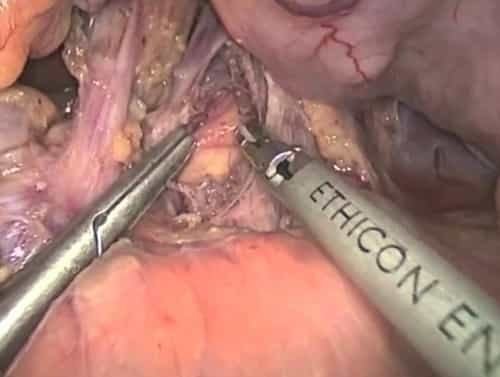
About 10% of patients have a conventional “open” operation, in which a large cut is made down the middle of the abdomen, typically with the support of among the vascular cosmetic surgeons. Patients who have this procedure may require to stay in the healthcare facility for 3 to 5 days for healing, and can generally go back to normal activities within 4 to six weeks.
What Type of Follow-up Care Is Needed After Median Arcuate Ligament Syndrome Surgery?
The majority of patients have a duplex ultrasound one month after surgery to make sure that there is no more compression of the median arcuate ligament. Some patients continue to have to construct of the celiac artery since of scar tissue that has developed. This generally does not trigger symptoms after surgery and can be treated with non-surgical strategies such as medications or, in uncommon cases, another celiac plexus block. Occasionally, other endovascular therapies might be needed. A little group of patients who have repeated episodes of MALS may be prospects for the 2nd effort at the release of the scar tissue. These patients, nevertheless, are at much higher risk (greater than 50%) of requiring an open operation (with the help of a vascular surgeon).