The ovaries are a fundamental part of the female reproductive system. Their job is twofold. They produce the hormonal agents, including estrogen, that set off menstruation. They likewise launch one egg each month for possible fertilization.
Right or left side abdominal pain around ovary
A number of different conditions, from cysts to tumors, can cause ovarian pain on left side or right side in ovary section. The ovaries lie in the lower abdominal area. That implies if you have ovarian pain, you’ll most likely feel it in your lower abdominal areas– below your belly button– and pelvis. It’s important to have any pelvic pain had a look at by your regular doctor or obstetrician/gynecologist. Several various conditions can cause it.
Pain in the ovaries can either be intense or chronic. Severe ovarian pain begins rapidly (over a couple of minutes or days) and disappears in a brief time period. Chronic ovarian pain generally starts more progressively. Then it last for several months.
Ovarian pain might be constant. Or it might reoccur. It might get worse with specific activities, such as exercise or urination. It can be so moderate that you don’t discover it. Or pain in the ovaries can be so severe that it disrupts daily life.
The approaches your doctor uses to identify ovarian pain will differ. They will be based on what the presumed cause may be. Regardless, your doctor will take a complete medical history, do a physical examination, and ask questions about your pain. The concerns might consist of:
- Where are you feeling the pain?
- When did it start?
- How often do you feel pain?
- Does an activity make the pain much better or even worse?
- How does it feel– mild, burning, achy, sharp?
- How does the pain impact your daily life?
Diagnostic tests, such as ultrasound and other types of imaging, can zero in on the cause of the pain. Here is a rundown of some possible causes of ovarian pain and how they are identified and alleviated.
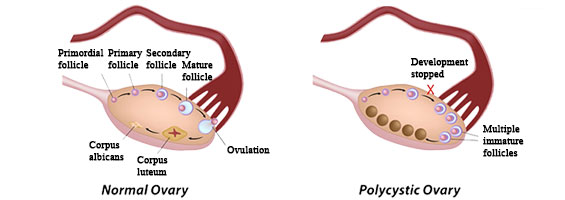
Ovarian Cysts
Cysts are fluid-filled sacs that can form in the ovaries. They are very common in women, especially during the childbearing years. Typically they form during the process of ovulation. It can happen when the egg is not released or when the sac– hair follicle– holding the egg does not dissolve after the egg is released. Ovarian cysts typically cause no symptoms and dissolve on their own. They can, though, create a dull ache or a sharp pain if one twists or ruptures.
Other symptoms of ovarian cysts:
- Irregular menstrual periods
- Pain during intercourse or bowel movements in left side or both
- Nausea or vomiting
- Feeling complete after consuming a percentage
- Bloating
How ovarian cysts are detected
- Pelvic test. This test might reveal a lump in the pelvic area.
- Ultrasound. This scan uses sound waves to produce a picture of the ovaries. This assists the doctor figure out the size and location of a cyst.
Treatment of ovarian cysts
- Careful waiting. Most ovarian cysts will go away by themselves. If you do not have any annoying symptoms, especially if you haven’t yet gone through menopause, your doctor may advocate “watchful waiting.” The doctor won’t treat you. Rather, the doctor might inspect you occasionally to see if there has been any change in your condition.
- Laparoscopy. This is a kind of surgery that uses little cuts and a small, lighted cam on the end of a plastic tube that’s placed into the abdominal area. A cosmetic surgeon can use tools on completion of television to eliminate some cysts. This strategy works for smaller cysts. Larger cysts, however, may need to be eliminated through a bigger incision in the abdominal area. This is finished with a method called laparotomy.
- Birth control pills. Birth control pills might eliminate the pain from ovarian cysts. They avoid ovulation. That, in turn, lowers the development of brand-new cysts.
Ovarian Tumors
Growths can form in the ovaries, just as they form in other parts of the body. They can be either noncancerous (benign) or cancerous (malignant).
Other symptoms of ovarian tumors
- Bloating or pressure in the left side of abdomen in the ovary area
- Immediate have to urinate
- Indigestion
- Diarrhea or constipation
- Anorexia nervosa
- Unintentional weight-loss or gain
How ovarian tumors are identified
- Computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (ANIMAL). These are detailed imaging scans that the doctor can use to discover ovarian tumors They enable the doctor to determine whether and how far the ovarian tumors have actually spread out.
- CA-125. This is a blood test to look for a protein that has the tendency to be greater in some (however not all) women with ovarian cancer. CA-125 isn’t really efficient as a screening test for ovarian cancer. However it can be examined in women with symptoms that might be brought on by ovarian cancer.
Treatment of ovarian tumors
- Laparotomy. This is surgery performed through an incision into the abdomen. The surgeon will get rid of as much of the growth as possible. The elimination of growth tissue is called debulking. If the growth is malignant and has actually spread, the specialist may likewise remove the ovaries, uterus, fallopian tubes, omentum (fat covering the intestinal tracts), and nearby lymph nodes.
- Chemotherapy. Chemotherapy includes drugs offered through a vein (IV), by mouth, or straight into the abdomen. The drugs eliminate cancer cells. Due to the fact that they eliminate regular cells also, chemotherapy medications can have side effects. These can consist of queasiness and vomiting, hair loss, kidney damage, and enhanced risk of infection. These side effects need to disappear after the treatment is stopped.
- Radiation. This treatment uses high-energy X-rays to eliminate or diminish cancer cells. Radiation is either delivered from outside the body, or positioned inside the body near the site of the growth. This treatment also can cause side effects. These can include inflamed skin, nausea, diarrhea, and fatigue. Radiation is seldom used to treat ovarian cancer.
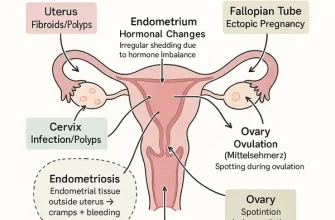
Ovarian Pain Caused by Endometriosis
Each month, the lining of the uterus builds up in preparation to nurture a growing fetus. When an egg is not fed, that lining sheds and is released from the body through menstruation. In some women, tissue like the lining of the uterus develops in other places in the body. This tissue swells and bleeds monthly. It has no place to shed, however, therefore it forms scar tissue and can be extremely painful.
Other symptoms of endometriosis
- Painful periods
- Pain during intercourse
- Heavy menstrual periods
- Infertility
How endometriosis is diagnosed
Ultrasound and MRI. These scans develop images of the ovaries to assist the doctor spot endometriosis
Laparoscopy. This procedure uses a thin lighted scope inserted into a small hole in the abdomen to enable the doctor to imagine the ovaries. The doctor may perhaps eliminate a small sample of tissue for biopsy.
Treatment of endometriosis
- Pain medications. Drugs such as ibuprofen (Advil, Motrin) can assist relieve a few of the discomfort of endometriosis.
- Contraceptive pill. The pill prevents the monthly accumulation of uterine tissue on the ovaries. This makes periods lighter and minimizes the symptoms of endometriosis.
- Gonadotropin-releasing hormone agonists (GnRH agonists). These drugs lower the quantity of the hormonal agent estrogen in the body. By slowing the growth of endometriosis, they limit its symptoms.
- Laparoscopy and laparotomy. These are surgical procedures that let the doctor remove endometriosis on the ovaries and other places. If the endometriosis is extensive, the doctor may recommend a hysterectomy. This procedure eliminates the uterus and often also the ovaries and fallopian tubes.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is an infection in the ovaries, uterus, or fallopian tubes. It is frequently caused by sexually transmitted conditions like gonorrhea or chlamydia. It is among the most typical causes of pelvic pain in women.
Other symptoms of PID
- Pain during sexual intercourse
- Fever
- Vaginal discharge that might have an odor
- Irregular menstrual bleeding
- Diarrhea
- Vomiting
- Fatigue
- Trouble urinating
How PID is identified
- Pelvic test. The exam will allow your doctor to search for any lumps, abnormal discharge, or inflammation in the pelvis.
- Blood and urine tests. These lab tests can assist recognize the infection. So can cultures of any discharge seen during a pelvic exam.
- Ultrasound. This test develops an image of the pelvic area so the doctor can see if the reproductive organs are enlarged. The doctor can likewise see if there is a pocket of infection known as an abscess.
- Laparoscopy. Periodically this procedure, which uses a thin lighted scope placed into a tiny hole in the abdominal area, is used to validate the diagnosis.
Treatment of PID
Antibiotics. These drugs are given by mouth or through an injection. They can eliminate the bacteria that are triggering PID. If you are taking antibiotics for PID, your sexual partner or partners need to also get alleviated. There is a high likelihood that your partner has the very same sexually transmitted infection.
Ovarian Residue Syndrome
Surgery to get rid of the uterus and ovaries is known as hysterectomy and oophorectomy. A bilateral salpingo oophorectomy is a procedure where both fallopian tubes and ovaries are eliminated. In unusual cases, a small piece of the ovary may mistakenly be left behind. The residue can grow and establish painful cysts.
Other symptoms of ovarian residue syndrome
- Pain during sexual intercourse
- Problem urinating
How ovarian residue syndrome is identified
Ultrasound, CT, and MRI. These scans develop pictures of the area. They help the doctor find the staying piece of ovary tissue.
Treatment of ovarian residue syndrome
Laparotomy or laparoscopy. These treatments are done to remove the staying piece or pieces of ovary.
Patients’ Stories
Story 1: Jessica’s Battle with Endometriosis
Jessica, a 32-year-old marketing executive, began experiencing sharp, intermittent pain in her lower abdomen. Assuming it was just the stress of her high-paced career, she initially dismissed the symptoms. However, as the pain intensified and became more frequent, she sought medical help. After a series of tests, Jessica was diagnosed with endometriosis, a condition where tissue similar to the one lining the inside of the uterus grows outside of it. This was the cause of her ovarian pain and explained the heavy periods and discomfort during intercourse she’d been experiencing. Jessica is now actively raising awareness about endometriosis and participates in support groups to help others who face similar challenges.
Story 2: Sophie’s Encounter with Ovarian Cysts
Sophie, a mother of two, woke up one morning to a dull, aching sensation in her lower right side. The discomfort quickly escalated to a level where she could barely stand up. Alarmed, she visited her doctor, who ordered an ultrasound. The images revealed several ovarian cysts—a fluid-filled sac within or on the surface of an ovary. Fortunately, Sophie’s cysts were benign and could be managed with medication, but the experience left her deeply aware of her health. She now volunteers for ovarian cancer screenings, encouraging other women to get regular check-ups.
Story 3: Linda’s Referred Pain Mystery
Linda, a retired schoolteacher, had been in good health until she started feeling recurring pain around her ovaries. Her primary care physician initially suspected ovarian-related issues, but further investigation indicated that the pain was referred from her gastrointestinal tract, particularly her gallbladder. After her gallbladder was treated, her ovarian pain subsided. Linda’s story sheds light on the complexity of diagnoses and the importance of thorough medical examinations. She now dedicates her time to a local health clinic, providing educational resources on various health conditions.
Story 4: Megan’s Mid-Cycle Discomfort
For Megan, a 27-year-old graphic designer, her monthly cycle brought more than just the typical discomfort. Mid-cycle, she would often experience sharp pain that would last for a few hours. After discussing this with her healthcare provider, Megan learned that she was experiencing mittelschmerz, a German term for “middle pain,” which occurs during ovulation. Understanding that this was a normal physiological process for some women brought Megan relief, both mentally and physically. She has since started a blog to document her experiences and to inform other women about the various aspects of reproductive health.