Stress Urinary Incontinence is a prevalent problem where the weakening of pelvic floor muscles causes the unintentional release of urine during actions like coughing, sneezing, laughing, or exercising. While it primarily affects women, men can also encounter this issue.
Symptoms
Stress Urinary Incontinence is characterized by a range of symptoms that can have a substantial impact on a person’s everyday routine. The main indication is the unintentional release of urine when engaging in physical actions that exert pressure on the bladder, such as coughing, sneezing, laughing, or exercising. Additional symptoms encompass:
- Urinary urgency: An abrupt and intense need to urinate, potentially leading to involuntary urine release if unable to reach a restroom quickly.
- Frequent urination: The need to urinate more often than usual, disrupting daily activities and sleep patterns.
- Nocturia: Waking up multiple times during the night to urinate.
- Urinary hesitancy: Difficulty initiating urination, feeling like the bladder is not fully empty.
- Urinary tract infections: Increased susceptibility to UTIs due to urine retention caused by incomplete emptying of the bladder.
Causes
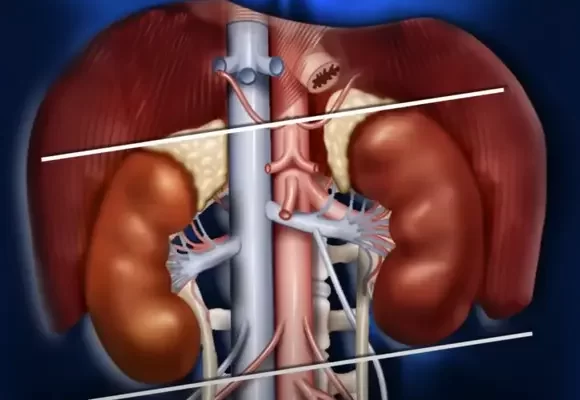
Stress Urinary Incontinence arises primarily from the weakening or damage of the muscles and tissues that support the bladder and urethra. This can happen as a result of various factors, including:
- Pregnancy and childbirth: Urinary incontinence may occur due to potential muscle and tissue damage caused by the pressure experienced by the pelvic floor throughout pregnancy and childbirth.
- Age-related changes: As people age, the muscles and tissues in the pelvic area may naturally weaken and lose their elasticity, leading to stress urinary incontinence.
- Menopause: During menopause, the decline in estrogen levels may lead to a weakening of the tissues and muscles in the pelvic region, which can result in urinary incontinence.
- Obesity: Being overweight can place extra strain on the bladder and muscles in the pelvic area, raising the chances of developing stress urinary incontinence.
- Chronic coughing: Recurring coughing caused by conditions like chronic bronchitis and asthma can exert pressure on the pelvic floor muscles, resulting in instances of urinary leakage.
- Certain medical procedures: Urinary incontinence may be caused by surgical interventions or medical treatments that affect the pelvic area, such as hysterectomy or radiation therapy, resulting in damage to the muscles and tissues.
Risk Factors
There are multiple factors that contribute to a person’s likelihood of experiencing stress urinary incontinence. These factors include:
- Gender: Women are more likely to experience stress urinary incontinence due to factors like pregnancy and childbirth that put pressure on the pelvic muscles, compared to men.
- Age: As individuals age, the likelihood of developing stress urinary incontinence increases. Due to the natural weakening of muscles and tissues in the pelvic area that occurs with age, the risk of experiencing urine leakage becomes greater.
- Obesity: Being overweight can increase the likelihood of stress urinary incontinence because it adds extra strain on the bladder and pelvic floor muscles.
- Smoking: Smoking can contribute to chronic coughing, which can strain the pelvic floor muscles and lead to urinary leakage.
- Family history: If a person has close relatives who have experienced stress urinary incontinence, their risk of developing the condition may be higher.
Diagnosis
To diagnose stress urinary incontinence, healthcare professionals may perform a variety of tests and assessments. Firstly, a comprehensive medical history will be obtained to understand the patient’s symptoms and potential underlying causes. A physical examination of the pelvic area will also be conducted to assess muscle strength and any signs of weakness or prolapse.
In addition, healthcare providers may use specific diagnostic tests, such as a urine analysis to rule out other urinary conditions, and urodynamic testing to evaluate bladder function and measure pressure changes during filling and emptying.
In some cases, imaging tests like ultrasound or cystoscopy may also be recommended to assess the bladder and urethra. These procedures allow for a closer examination of the structures involved in urinary function.
By conducting a thorough evaluation, healthcare professionals can accurately diagnose stress urinary incontinence and determine the most appropriate treatment options for the individual. It is important to consult with a healthcare provider if experiencing symptoms of stress urinary incontinence to undergo the necessary diagnostic procedures.
Treatment Methods
Treatment for stress urinary incontinence may involve both non-surgical and surgical options, depending on the severity of the condition and the individual’s preferences.
Non-surgical interventions include pelvic floor muscle exercises, also known as Kegel exercises, which aim to strengthen the muscles that support the bladder and urethra. Biofeedback, which provides visual or auditory cues to facilitate proper muscle contractions, may be used alongside Kegel exercises to enhance their effectiveness.
In some cases, healthcare professionals may recommend the use of vaginal pessaries, which provide support to the urethra and prevent leakage.
For more severe cases, surgical interventions such as sling procedures or vaginal mesh implants may be considered. These procedures help support the urethra and reduce the symptoms of stress urinary incontinence.
Prevention
While stress urinary incontinence cannot always be completely prevented, there are steps that individuals can take to reduce the risk of developing or worsening the condition. The aim of these precautionary actions is to enhance the muscles of the pelvic floor and uphold a lifestyle that promotes good health. Here are a few approaches that could be beneficial:
- Pelvic floor exercises: Engaging in Kegel exercises on a consistent basis can aid in building up the muscles that provide support to the bladder and urethra, thereby lessening the likelihood of experiencing stress urinary incontinence.
- Maintain a healthy weight: Being overweight can cause more strain on the muscles in the pelvic floor, which can result in a higher chance of experiencing urinary leakage. Keeping a healthy weight by engaging in consistent physical activity and following a well-rounded diet can assist in avoiding stress urinary incontinence.
- Avoid smoking: Smoking increases the likelihood of experiencing stress urinary incontinence because it can weaken the muscles in the pelvic floor. Ceasing smoking can enhance control over the bladder and lessen the effects of incontinence.
- Stay hydrated: It is important to stay properly hydrated to prevent urinary tract infections, which can contribute to urinary incontinence. Drinking enough water throughout the day can help maintain bladder health.
- Avoid bladder irritants: Certain foods and drinks, such as caffeine, alcohol, and spicy foods, can irritate the bladder and worsen urinary incontinence symptoms. Limiting or avoiding these irritants can help prevent leakage.
- Treat chronic coughing: Chronic coughing can put strain on the pelvic floor muscles and increase the risk of stress urinary incontinence. Treating underlying respiratory conditions and managing coughing can help prevent and manage the condition.
By adopting these preventive measures, individuals can minimize their risk of developing stress urinary incontinence and improve their overall bladder control. It is important to consult with a healthcare professional for personalized advice and guidance on specific preventive strategies.
Lifestyle
Lifestyle plays a crucial role in managing stress urinary incontinence. Simple modifications in daily activities can significantly improve bladder control and reduce incontinence episodes. Here are some lifestyle tips to consider:
- Healthy Diet: Consuming a well-balanced diet rich in fiber can prevent constipation, which contributes to bladder problems. It is essential to include fresh fruits, vegetables, whole grains, and lean proteins in the diet.
- Fluid Intake: It is important to maintain hydration levels by drinking adequate amounts of water throughout the day. However, excessive fluid intake before bedtime should be avoided to minimize nighttime bathroom visits.
- Regular Bathroom Habits: Developing a consistent bathroom routine by emptying the bladder at regular intervals can help in preventing urinary leakage. Timed voiding techniques can train the bladder and improve control.
- Weight Management: Maintaining a healthy weight can help reduce pressure on the bladder and pelvic floor muscles. Regular exercise and portion control can aid in weight management.
- Avoiding Heavy Lifting: Engaging in strenuous activities like weightlifting or carrying heavy objects can put pressure on the pelvic floor muscles, potentially leading to stress urinary incontinence. To prevent this condition, it is advisable to reduce or completely avoid such activities.
Improving bladder control and the overall quality of life can be achieved by adopting these lifestyle changes. It is crucial to seek personalized advice and guidance from a healthcare professional when dealing with stress urinary incontinence.