Chronic pyelonephritis is continuing pyogenic infection of the kidney that occurs virtually specifically in patients with major anatomic problems. Symptoms consist of fever, malaise, and flank pain. Medical diagnosis is with urinalysis, culture, and imaging tests. Treatment is with antibiotics and correction of any structural disorders.
Reflux of infected urine into the kidney pelvis is the typical system. Causes include obstructive uropathy, struvite calculi, and, the majority of frequently, vesicoureteral reflux (VUR).
Pathologically there is atrophy and calyceal defect with overlying parenchymal scarring. Chronic pyelonephritis might progress to chronic kidney disease. Patients with chronic pyelonephritis may have recurring foci of infection that might predispose to bacteremia or, among kidney transplant patients, seed the urinary tract and transplanted kidney.
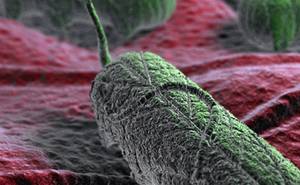
Xanthogranulomatous pyelonephritis (XPN) is an uncommon variation that appears to represent an unusual inflammatory response to infection. Giant cells, lipid-laden macrophages, and cholesterol clefts represent the yellow color of the infected tissue. The kidney is enlarged, and perirenal fibrosis and adhesions to adjacent retroperitoneal structures are common. The condition is almost always unilateral and most often occurs in middle-aged women with a history of persistent UTIs. Long-term urinary tract obstruction (typically by a calculus) and infection increase risk. The most typical pathogens are Proteus mirabilis and Escherichia coli.
Symptoms and Signs
Symptoms and signs of chronic pyelonephritis are typically unclear and irregular. Some patients have fever, flank or abdominal pain, despair, or anorexia. In XPN, a unilateral mass can normally be palpated.
Medical diagnosis
- Urinalysis and urine culture
- Imaging
Chronic pyelonephritis is believed in patients with a history of frequent UTIs and acute pyelonephritis. Nevertheless, most patients, except for children with VUR, do not have such a history. Sometimes the diagnosis is presumed due to the fact that normal findings are by the way noted on an imaging study. Symptoms, due to the fact that they are unclear and nonspecific, might not recommend the medical diagnosis.
Urinalysis and urine culture and generally imaging tests are done. Urinary sediment is normally little, but kidney epithelial cells, granular casts, and periodically WBC casts exist. Proteinuria is usually present and can be in the nephrotic variety if VUR causes comprehensive renal damage. When both kidneys are involved, defects in concentrating ability and hyperchloremic acidosis might appear prior to significant azotemia takes place. Urine culture may be sterilized or favorable, usually for gram-negative organisms.
Preliminary imaging is generally with ultrasonography, helical CT, or IVU. The hallmark of chronic pyelonephritis (typically with reflux or obstruction) on imaging is classically a big, deep, segmental, coarse cortical scar generally encompassing one or more of the kidney calyces. The upper pole is the most typical website. Kidney cortex is lost, and the kidney parenchyma thins. Uninvolved kidney tissue might hypertrophy locally with segmental enhancement. Ureteral dilation may exist, showing the changes caused by chronic severe reflux. Comparable changes can accompany urinary tract TB (see Genitourinary TB).
In XPN, urine cultures usually grow P. mirabilis or E. coli. CT imaging is done to identify calculi or other obstruction. Imaging shows an avascular mass with a variable degree of extension around the kidney. In some cases, to distinguish cancer (eg, kidney cell carcinoma), biopsy may be required, or tissue gotten rid of throughout nephrectomy can be analyzed.
Diagnosis
The course of chronic pyelonephritis is exceptionally variable, but the disease generally advances really slowly. A lot of patients have sufficient kidney function for ≥ 20 yr after onset. Regular worsenings of intense pyelonephritis, although controlled, generally additional deteriorate kidney structure and function. Continued obstruction predisposes to or perpetuates pyelonephritis and increases intrapelvic pressure, which damages the kidney directly.
Treatment
If obstruction can not be removed and frequent UTIs are common, long-term treatment with antibiotics (eg, trimethoprim/sulfamethoxazole, trimethoprim, a fluoroquinolone, nitrofurantoin) works and may be needed forever. Complications of uremia or hypertension have to be dealt with appropriately.
For XPN, a preliminary course of antibiotics ought to be provided to manage regional infection, followed by en bloc nephrectomy with elimination of all involved tissue.
Patients undergoing kidney transplant who have chronic pyelonephritis may require nephrectomy prior to the transplant.
Key Points
- Chronic pyelonephritis normally influences patients predisposed to urinary reflux into the kidney hips (eg, by VUR, obstructive uropathy, or struvite calculi).
- Suspect chronic pyelonephritis if patients have recurrent acute pyelonephritis, however the medical diagnosis is often first presumed based upon incidental findings on imaging.
- Acquire an imaging research study (ultrasonography, helical CT, or IVU).
- If obstruction can not be alleviated, contemplate long-term antibiotic prophylaxis.