Having Endometrial Hyperplasia can present difficulties, but there are ways to handle the symptoms and receive support. We will give an introduction to endometrial hyperplasia and how it affects daily life, along with different treatment choices.
It will also explore techniques for managing the symptoms, alternative therapies, and lifestyle changes that can enhance overall well-being.
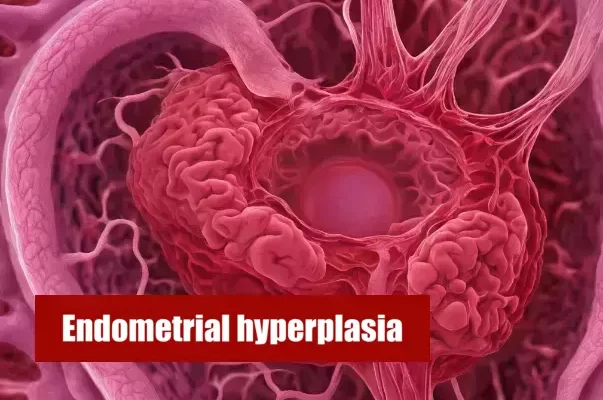
Overview of Endometrial hyperplasia
Endometrial hyperplasia is a medical condition where the lining of the uterus, called the endometrium, experiences abnormal growth. This overgrowth can cause irregularities in menstruation and can raise the chances of developing endometrial cancer. It is crucial for those with endometrial hyperplasia to comprehend the implications of this condition on their everyday life, in order to successfully handle their symptoms and obtain the necessary medical attention.
How it affects daily life
Endometrial hyperplasia can significantly impact daily life for those who are affected by it. The symptoms, such as abnormal bleeding and pelvic pain, can cause discomfort and inconvenience. The condition may also affect a person’s emotional well-being and lead to anxiety or stress. Managing these symptoms and maintaining a normal routine can be challenging for individuals living with endometrial hyperplasia.
Causes and symptoms of Endometrial Hyperplasia
Endometrial hyperplasia is caused by an excess growth of cells in the lining of the uterus, known as the endometrium. This can be triggered by hormonal imbalances, obesity, certain medications, or polycystic ovary syndrome (PCOS). Symptoms may include abnormal uterine bleeding, such as heavy or prolonged periods, pelvic pain, and in some cases, difficulty getting pregnant. It is important to seek medical attention if you experience any of these symptoms.
Different types of Endometrial Hyperplasia
There are different types of Endometrial Hyperplasia, including simple hyperplasia without atypia, complex hyperplasia without atypia, simple hyperplasia with atypia, and complex hyperplasia with atypia. Each type varies in the extent of abnormal cell growth and the potential for developing into cancer. It is important for individuals diagnosed with Endometrial Hyperplasia to understand their specific type and its implications for their condition.
Diagnosis
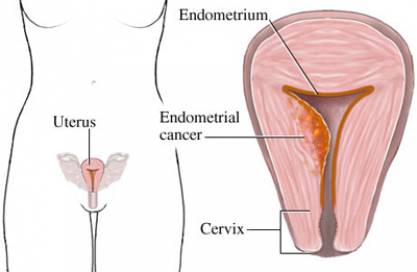
Diagnosis of endometrial hyperplasia typically involves a combination of medical history review, physical examination, and tests. The main diagnostic tool is an endometrial biopsy, where a sample of tissue from the lining of the uterus is collected for analysis. Other tests such as ultrasounds or imaging studies may also be used to assess the thickness of the uterine lining. This process allows healthcare professionals to accurately identify and determine the severity of endometrial hyperplasia.
Treatment options available
- Hormonal therapy: This involves the use of medications such as progestin to regulate the growth of the endometrium.
- Endometrial ablation: This procedure uses heat or laser to remove the excess tissue in the uterus.
- Hysterectomy: In severe cases, removing the uterus may be recommended as a last resort treatment option.
- Regular monitoring: Doctors may suggest frequent follow-ups and biopsies to track the progression of the condition and make necessary adjustments to treatment plans.
Coping With Endometrial Hyperplasia Symptoms
To cope with the symptoms of endometrial hyperplasia, there are various techniques and strategies that can help individuals manage their discomfort. These techniques may include pain management techniques, such as using heat or over-the-counter pain medications, as well as making dietary changes and adopting a healthy lifestyle.
List of the pain management techniques
Pain management techniques for individuals with endometrial hyperplasia may include nonsteroidal anti-inflammatory drugs (NSAIDs) to alleviate menstrual pain. Heating pads or hot water bottles can provide relief by reducing muscle cramps.
Additionally, some individuals may find relief through gentle exercise or physical therapy. It is important to consult with a healthcare professional to determine the best pain management plan for each individual’s specific needs.
Dietary changes and lifestyle tips
Dietary changes and lifestyle tips can play a crucial role in managing endometrial hyperplasia. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can provide essential nutrients.
Limiting the intake of processed foods, sugar, and caffeine may also be beneficial. And definitely, quitting alcohol and smoking should be mandatory for you anyway.
Additionally, maintaining a healthy weight through regular exercise and getting enough rest can help alleviate symptoms. It is recommended to consult with a healthcare professional or nutritionist for personalized dietary advice.
Alternative Therapies
Alternative therapies have gained popularity as potential treatments for endometrial hyperplasia. While there is limited scientific evidence to support their effectiveness, some individuals have reported positive results in managing symptoms. It is important to consult with a healthcare professional before considering any alternative therapy, as they can provide guidance and ensure safety.
Effectiveness in treating Endometrial Hyperplasia
When it comes to treating endometrial hyperplasia, the effectiveness of different therapies and treatments may vary depending on the individual. While some may find relief and improvement with conventional treatments such as hormone therapy or surgery, others may explore alternative therapies like herbal remedies. It is important for patients to work closely with their healthcare providers to find the most effective treatment plan for their specific condition.
Making Lifestyle Changes
Stress management techniques and exercises can greatly benefit individuals living with endometrial hyperplasia. Incorporating regular physical activity into daily routines, such as walking or gentle stretching, can aid in managing symptoms and improving overall quality of life for those with endometrial hyperplasia. Making these lifestyle changes can contribute to a better sense of control and empowerment for patients.
Stress Management techniques
To effectively manage stress associated with endometrial hyperplasia, it is important to incorporate stress management techniques into daily life. These can include practicing relaxation exercises and enjoyment like reading, seeking support from loved ones, and making time for self-care activities that reduce stress and promote overall well-being.
Implementing these strategies can help individuals cope with the emotional and physical challenges of living with endometrial hyperplasia.
Exercises for Endometrial Hyperplasia patients
Exercises can play a vital role in managing the symptoms of Endometrial Hyperplasia. Engaging in regular physical activity can also enhance mood and reduce stress levels, contributing to a better quality of life for individuals with Endometrial Hyperplasia.
Conclusion
In conclusion, living with Endometrial Hyperplasia can be challenging, but there are coping strategies and support available to help manage the symptoms and improve quality of life. By understanding the condition, seeking appropriate medical care, and implementing lifestyle changes, individuals with Endometrial Hyperplasia can find hope and perseverance. It is important to remember that resources for further help and support are readily available for those in need.
Perseverance and hope for Endometrial Hyperplasia patients
Endometrial Hyperplasia can be a challenging condition to live with, but it’s important for patients to remember that there is hope and the potential for improvement. By persevering through the symptoms and following the recommended treatment plan, Endometrial Hyperplasia patients can find relief and regain control over their daily lives. With the support of medical professionals, loved ones, and online communities, they can navigate this journey with resilience and hope for a better future.
Patients’ Stories
The Story of Samantha: A Journey of Awareness and Proactive Treatment
Samantha, a 42-year-old real estate agent, began experiencing irregular menstrual cycles and abnormally heavy bleeding. Never overly concerned about her health before, these changes prompted her to consult her doctor. After an ultrasound and a biopsy, she was diagnosed with endometrial hyperplasia. The condition was a wake-up call for Samantha, who realized that her sedentary lifestyle and recent weight gain might have played a role.
Fortunately, Samantha’s type of hyperplasia was without atypia, meaning the risk of it developing into cancer was low. Her gynecologist recommended a conservative approach with progestogen therapy, which Samantha followed diligently. Within a few months, her menstrual cycles normalized, and a follow-up biopsy showed resolution of the hyperplasia. Samantha’s story is a testament to how early detection and treatment can lead to a positive outcome. Additionally, motivated by her condition, Samantha embraced healthier habits, including regular exercise and a balanced diet.
Jennifer’s Battle with Persistent Symptoms and Intervention
Jennifer, a 35-year-old graphic designer with a passion for her work, often neglected her health due to her busy schedule. When she started having persistent abnormal bleeding, she brushed it off as stress-related until the symptoms became too disruptive to ignore. Upon seeking medical advice, Jennifer discovered she had endometrial hyperplasia, and her relentless symptoms were indicative of the condition’s progression.
She underwent a more aggressive treatment due to the severity of her symptoms. Her gynecologist prescribed a higher dosage of progestogen and monitored her response closely. The road to recovery wasn’t smooth, and Jennifer sometimes struggled with the side effects of the treatment. However, after several months, her persistence paid off as her symptoms abated, and the follow-up tests showed no signs of hyperplasia. Jennifer’s experience underscored the importance of not dismissing persistent health issues and the effectiveness of following through with a treatment plan, even when it’s challenging.
Ursula’s Confrontation with a Scare and Lifestyle Changes
In her late 50s, Ursula, a retired teacher, faced a significant health scare when she was diagnosed with atypical endometrial hyperplasia. She learned that this condition carried a higher risk of developing into cancer if left untreated. Ursula’s initial reaction was one of anxiety, but she quickly channeled her energies into understanding and combating the disease.
Her doctors decided that a more assertive approach was necessary due to the atypia. Besides medical treatment with progestins, Ursula was counseled about the importance of lifestyle modifications, especially weight management to reduce her body’s estrogen production. Determined to improve her prognosis, she adopted a healthier diet and began a supervised exercise regimen. Over time, not only did Ursula’s hyperplasia resolve, but she also felt more energetic and overall healthier than she had in years. Her story is a powerful reminder of the body’s ability to heal when supported by medical care and positive lifestyle choices.