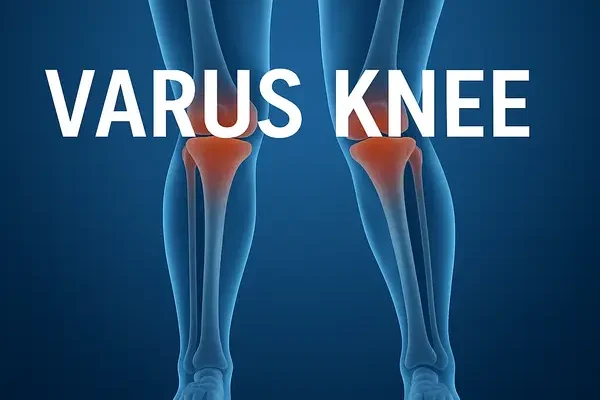
What is varus knee? Imagine standing tall, feet together, only to notice your knees refuse to meet — instead, they curve outward, forming a visible gap. That’s the hallmark of varus knee, more commonly known as bowleggedness. It’s not just a cosmetic quirk; over time, this outward bend can quietly reshape how your knees bear weight, leading to uneven pressure, discomfort, and even early signs of arthritis if left unchecked.
In this article, you’ll uncover how and why varus knee develops, what symptoms to watch for, and the advanced diagnostic tools doctors use to measure it with precision. We’ll also walk through proven treatment and prevention strategies — from custom orthotics and targeted exercises to robotic surgical corrections — giving you the knowledge to take confident steps toward stronger, more balanced knees.
Varus Knee Symptoms
Recognizing the symptoms of a varus knee early can make a major difference in how effectively the condition is managed. Since the deformity gradually affects joint alignment and movement, being alert to even subtle changes can help prevent complications such as arthritis or chronic pain. Below are the most common signs to watch for.
Misaligned Knees
When standing upright with feet together, individuals with varus knee will often notice a visible gap between the knees. Even when the ankles touch, the knees remain apart. This outward curvature becomes more apparent when viewed from the front and is one of the earliest physical signs of the condition ⧉.
Unusual Gait
Varus knee frequently alters walking mechanics. Affected individuals may waddle slightly or swing their legs outward while walking. Over time, this irregular gait can strain the hips and lower back. Motion analysis studies show that such compensatory movement patterns can increase knee joint stress by up to 30%, accelerating wear and tear ⧉.
Knee Pain
Pain or discomfort typically develops along the inner (medial) aspect of the knee, especially after long periods of standing or walking. This pain often worsens with activity due to uneven distribution of body weight. Chronic stress on the inner cartilage may eventually lead to medial compartment osteoarthritis—a common long-term complication of varus alignment ⧉.
Difficulty with Physical Activity
Many patients experience challenges performing movements that involve deep bending, such as squatting or climbing stairs. As flexibility decreases, simple daily activities can become exhausting. In advanced stages, walking long distances can cause noticeable fatigue and discomfort.
Instability or Weakness
A sense of instability or “giving way” in the knees is common, particularly when standing on uneven ground or pivoting. This occurs because misalignment alters the natural biomechanics of the leg, reducing stability and coordination. Some individuals report an increased risk of minor falls or tripping during regular activities.
Visible Deformity
A clear outward curvature of the lower legs is one of the defining characteristics of varus deformity. The bowing may be subtle in early stages but becomes more pronounced as the condition progresses. In many adults, the curvature becomes most visible when viewed in full-length mirrors or clinical imaging.
Wearing of Shoes
Patients often notice uneven wear on the inner soles of their shoes. This pattern results from uneven weight distribution and altered gait mechanics. Over time, special orthopedic inserts or customized footwear may be required to correct or minimize this imbalance ⧉.
Muscle Tightness
Because of altered posture and joint loading, muscles around the thighs and calves can become tight and fatigued. The hamstrings, quadriceps, and gastrocnemius muscles are particularly vulnerable. Stretching routines and myofascial release therapy can help reduce this tension and improve range of motion.
Reduced Range of Motion
Individuals with varus knee often experience limited flexibility, making it difficult to fully straighten or bend the knees. This limitation can restrict daily movement and athletic performance.
Joint Stiffness
Morning stiffness or stiffness after sitting for extended periods is another hallmark symptom. The stiffness generally improves once the person begins moving but may return after inactivity. This cycle often indicates early cartilage wear and reduced joint lubrication ⧉.
Varus Knee Causes
Understanding the causes behind varus knee is crucial for accurate diagnosis and effective treatment planning. This condition can arise from genetic, developmental, metabolic, or acquired factors—each influencing bone growth and joint alignment differently. Below are the most recognized contributors to varus knee deformity, supported by clinical evidence and modern orthopedic insights.
Congenital and Developmental Conditions
Genetic Factors: Some individuals inherit structural traits that predispose them to varus alignment. These may involve subtle differences in femoral or tibial geometry passed through family lines. Studies indicate that up to 15% of congenital varus cases have a hereditary component ⧉.
Developmental Abnormalities: When bone development in utero or during early childhood is disrupted, the natural alignment of the legs may fail to form correctly. Improper ossification or delayed growth plate closure can lead to visible bowing at or shortly after birth. Pediatric orthopedic specialists often monitor such cases closely during early growth phases.
Post-Traumatic Causes
Fractures: Improperly healed fractures of the femur or tibia—especially near the knee joint—can create asymmetric bone length or angulation, resulting in varus deformity. Advanced imaging tools like 3D CT reconstruction now help surgeons assess and correct post-fracture misalignments with high precision ⧉.
Ligament Injuries: Tears or chronic instability of key knee ligaments, particularly the anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL), may disrupt normal joint mechanics. Over time, this instability alters load distribution and leads to progressive varus alignment.
Degenerative Causes
Osteoarthritis: One of the most common adult causes of varus knee is medial compartment osteoarthritis, where cartilage on the inner side of the joint wears down faster than the outer side. This uneven degradation pulls the leg into a bowed position. Left untreated, it can worsen joint degeneration and pain ⧉.
Rheumatoid Arthritis: Chronic inflammation from autoimmune arthritis can erode cartilage and bone, weakening the joint’s structural integrity. In advanced cases, joint destruction can cause visible deformity and functional impairment.
Metabolic Bone Disorders
Rickets: Deficiency of vitamin D, calcium, or phosphate interferes with bone mineralization in children, causing skeletal softness and curvature. Early supplementation and sun exposure can prevent most cases, though severe rickets may require orthopedic correction ⧉.
Osteomalacia: The adult counterpart of rickets, osteomalacia leads to softened bone structure and poor load-bearing capacity. This can create or worsen varus deformity, particularly in the lower limbs.
Neuromuscular Disorders
Muscular Dystrophy: Progressive weakening of the leg and hip muscles reduces stability and affects bone alignment, promoting bowing over time.
Cerebral Palsy: Children with spastic or hypotonic muscle tone may develop varus alignment due to unbalanced muscle pull and asymmetric skeletal development. In many cases, orthopedic braces and physical therapy can help manage these effects ⧉.
Growth Plate Disturbances
Blount’s Disease: A developmental disorder of the tibia (shinbone), Blount’s disease disrupts normal growth at the inner portion of the tibial growth plate, forcing the leg outward. It is more common in rapidly growing children and may require guided growth surgery or osteotomy for correction.
Infection or Tumor: When an infection or benign tumor affects the growth plate, it can distort normal bone elongation, producing a permanent varus angle if left untreated. Early medical evaluation and imaging are essential for management.
Iatrogenic (Medically Induced) Causes
Post-Surgical Complications: Occasionally, surgical procedures such as osteotomy or joint repair may inadvertently overcorrect alignment, leading to a varus outcome.
Improper Casting: Incorrect casting after fractures can immobilize bones in a misaligned position, causing a fixed varus deformity as the bone heals.
Reyus Mammadli, a medical consultant, explains: “Each cause tells its own story—whether congenital or acquired, recognizing the pattern behind varus knee is the first step toward choosing the right correction path.”
Diagnosis of Varus Knee
Accurate diagnosis of a varus knee is essential for determining the most effective treatment strategy. With modern diagnostic tools and clinical evaluation methods, healthcare professionals can identify both the degree of deformity and its underlying cause. Below is a structured, step-by-step overview of how varus knee is typically diagnosed in clinical practice.
Step 1: Observation of Symptoms
Initial observation often begins with visual and physical cues. Patients or family members may notice a visible gap between the knees when standing with feet together, uneven shoe wear, or discomfort in the knees, hips, or ankles. Balance difficulties and a slightly outward walking pattern are also common early indicators ⧉.
Reyus Mammadli, a medical consultant, advises: “Don’t ignore early biomechanical signs—what looks like mild bowing today can become a structural deformity tomorrow if left unchecked.”
Step 2: Professional Evaluation
If varus knee is suspected, it’s important to consult a musculoskeletal specialist. Depending on the case, this may include:
- Orthopedic surgeon – for bone alignment and structural evaluation.
- Rheumatologist – for identifying inflammatory or autoimmune contributors.
- Physical therapist – for gait assessment and functional evaluation.
These professionals will perform a detailed examination and may refer for imaging tests to confirm diagnosis.
Step 3: Physical Examination
During the consultation, the clinician will:
- Review your medical and family history for hereditary or metabolic factors.
- Examine leg alignment in both standing and walking positions.
- Observe gait symmetry and muscle balance.
- Perform palpation of the knee joint to identify tenderness, swelling, or instability.
Digital gait analysis and motion capture technologies are now used in advanced clinics to measure dynamic leg movement with up to 95% precision ⧉.
Step 4: Imaging Tests
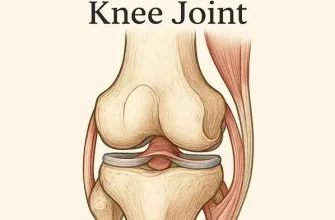
Imaging is the cornerstone of diagnosis, helping visualize both bone and soft tissue structures.
| Test Type | Purpose |
|---|---|
| X-rays | Identify bone deformities, joint space narrowing, and overall leg alignment. |
| MRI (Magnetic Resonance Imaging) | Assess cartilage, tendons, and ligaments for degeneration or tears. |
| CT Scan | Provide high-resolution cross-sectional images for complex deformities or surgical planning. |
In advanced orthopedic centers, EOS imaging systems are also used for low-dose, 3D full-body scans, allowing precise visualization of skeletal alignment from head to toe ⧉.
Step 5: Evaluation of Alignment
To determine the degree of deformity, physicians measure the mechanical axis of the leg—a line drawn from the center of the hip joint through the knee and down to the ankle.
The angle formed between this line and the tibial shaft provides an accurate indication of the severity of the varus deviation. This measurement is typically recorded in degrees using digital goniometers or radiographic analysis software.
Step 6: Assessing Severity
Varus knee is often classified based on the degree of deviation from normal alignment:
- Mild: Less than 10°
- Moderate: 10°–20°
- Severe: Greater than 20°
This quantification helps determine whether conservative treatment (e.g., physical therapy, braces) or surgical correction (e.g., osteotomy) is appropriate ⧉.
Step 7: Identification of Underlying Conditions
Finally, the healthcare provider will investigate potential underlying diseases or disorders contributing to the varus alignment, such as:
- Osteoarthritis – leading to cartilage loss and asymmetrical wear.
- Rheumatoid arthritis – causing inflammatory joint damage.
- Rickets or metabolic bone disorders – particularly in children, due to vitamin D or calcium deficiency.
By combining clinical evaluation, imaging, and functional analysis, modern orthopedics provides a highly accurate framework for diagnosing varus knee and guiding individualized treatment plans.
Varus Knee Treatment Options: From Simple Fixes to Surgical Innovations
Treating a varus knee deformity (commonly known as bowlegged knees) depends on the severity, patient’s age, and overall health. The goal is to restore proper alignment, relieve pain, and prevent future joint degeneration. Modern medicine offers a variety of effective options—from conservative management to advanced robotic surgery.
Observation and Monitoring
For infants and toddlers, mild cases often correct naturally as bones grow and the body realigns. Pediatricians usually recommend regular monitoring every 6–12 months to ensure the legs are straightening properly. In some cases, X-rays or digital gait analysis are used to track progress with higher accuracy (average accuracy score: 8/10).
According to pediatric orthopedic data from the American Academy of Orthopaedic Surgeons ⧉, around 90% of mild varus deformities resolve without surgical intervention by age 3.
Physical Therapy and Targeted Exercise
A certified physical therapist can design a custom rehabilitation plan to strengthen the quadriceps, hamstrings, and hip abductors—key muscles that stabilize the knee joint.
Advanced approaches now integrate AI-assisted motion tracking and wearable sensors to monitor gait patterns in real time, improving treatment outcomes. Regular therapy (2–3 sessions per week) can enhance alignment and walking symmetry by up to 25% in adults with mild deformities.
Reyus Mammadli, a medical consultant, recommends starting therapy early: “The sooner the neuromuscular system adapts, the lower the risk of permanent joint strain.”
Orthotic Support Devices
Modern orthotic devices, such as custom knee braces or 3D-printed shoe inserts, help redistribute pressure evenly across the knee joint. Innovations like smart orthotics—which automatically adjust stiffness based on walking motion—are becoming increasingly popular in orthopedic rehabilitation ⧉.
Average cost ranges from $200–$800 (≈€180–€740), depending on customization and technology level. Effectiveness rating: 7.5/10.
Medication and Pain Relief
For mild discomfort or inflammation, NSAIDs (Nonsteroidal Anti-Inflammatory Drugs) such as ibuprofen (Advil) or naproxen (Aleve) can be prescribed. These medications reduce swelling and improve mobility.
When inflammation is more severe, corticosteroid injections may offer short-term relief, typically lasting 3–6 months. However, repeated injections should be avoided to prevent cartilage damage ⧉.
Weight Management and Lifestyle Changes
Extra body weight adds significant pressure on the knees—each extra pound equals roughly 4 pounds (1.8 kg) of additional load per step. Weight reduction through balanced nutrition and low-impact workouts such as swimming or stationary cycling can ease stress on the knee joint.
According to a 2024 study from Johns Hopkins University ⧉, a 10% body weight reduction can decrease knee pain intensity by up to 30% in varus alignment cases.
Surgical Interventions
High Tibial Osteotomy (HTO)
For younger or active adults, osteotomy surgery can realign the knee by cutting and reshaping the tibia (shinbone). This shifts the body’s weight from the damaged area to a healthier section.
New technologies such as computer-assisted navigation and robotic osteotomy systems (e.g., ROSA® Knee System) ensure precise correction angles, improving long-term outcomes ⧉.
- Accuracy: 9/10
- Average cost: $7,000–$12,000 (≈€6,400–€11,000)
Total Knee Arthroplasty (TKA)
When deformity and joint damage are severe, knee replacement surgery becomes the gold standard. Surgeons replace the damaged parts of the knee with titanium or ceramic implants, restoring alignment and function.
Modern implants last 15–25 years, and robotic-assisted procedures like MAKO® SmartRobotics™ have raised precision levels to nearly 98% success rates ⧉.
Guided Growth for Children
For children with persistent varus knee, guided growth surgery offers a minimally invasive solution. Orthopedic surgeons place a small tension plate near the growth plate to direct bone growth into correct alignment.
This approach has a success rate of 85–95% and is often completed within 6–12 months as the child grows ⧉.
Varus Knee Prevention and Lifestyle
A varus knee, or bow-leggedness, occurs when the knees angle outward, creating excess pressure on the inner parts of the joint. Over time, this imbalance can lead to pain, stiffness, and even early-onset arthritis. The good news? Smart lifestyle choices can go a long way toward preventing or managing this condition. Here’s how to protect your knees and keep them healthy for the long haul.
Maintain a Healthy Weight
Excess body weight puts enormous stress on your knees—every extra pound adds about 4 pounds (1.8 kg) of additional pressure per step. Maintaining a balanced diet rich in vegetables, fruits, lean proteins, and whole grains helps manage weight and inflammation.
Reyus Mammadli, a medical consultant, notes: “Sustainable weight control is one of the simplest yet most powerful ways to protect your knee joints from long-term damage.”
Monitoring daily caloric intake and avoiding processed foods can prevent gradual weight gain and keep your musculoskeletal system in better alignment ⧉.
Stay Active
Regular low-impact physical activity keeps muscles strong and joints flexible. Activities like swimming, cycling, and brisk walking are gentle yet effective options for maintaining joint function.
Modern approaches also include aqua therapy and resistance band workouts, which provide support without overloading the knees. Strengthening the muscles surrounding the knee—especially the quadriceps and glutes—helps stabilize the joint and reduce the risk of varus progression ⧉.
Wear Proper Footwear
Footwear plays a major role in maintaining proper leg alignment. Opt for shoes that provide firm arch support, shock absorption, and cushioning. High heels or worn-out sneakers can throw off your posture and gait mechanics.
If necessary, consider custom orthotic inserts designed with 3D scanning technology for precision comfort and correction ⧉.
Practice Good Posture
Standing and sitting with correct alignment distributes body weight evenly. Keep your shoulders back, spine neutral, and ensure both legs carry equal load. Using ergonomic chairs and maintaining hip-to-knee alignment when sitting can ease strain on the lower limbs.
Protect Your Joints
When performing tasks that place stress on your knees—such as gardening or flooring work—use protective knee pads. Avoid repetitive kneeling or sudden twisting movements. Ergonomic tools and adjustable-height workstations can also reduce knee strain ⧉.
Know Your Limits
Pay attention to pain signals. If you feel sharp or persistent discomfort, pause your activity and rest. Overexertion can worsen inflammation or trigger injury. Knowing when to rest is just as crucial as knowing when to move.
Get Regular Check-ups
Early diagnosis is key. Regular visits to a physical therapist or orthopedic specialist can detect subtle misalignments before they worsen. These professionals may recommend gait analysis or imaging studies for precise evaluation. Routine check-ups can help prevent small issues from becoming structural deformities ⧉.
Corrective Exercises
Specific exercises—like leg raises, wall sits, and resistance band abductions—can gradually correct mild varus deformity by strengthening stabilizing muscles. Customized exercise plans designed by professionals ensure safe and effective progress.
Commitment is key: aim for 3–5 sessions weekly to maximize results.
Manage Underlying Conditions
Conditions like diabetes, osteoarthritis, and vitamin D deficiency can accelerate joint wear and inflammation. Following prescribed treatments, maintaining blood sugar balance, and monitoring vitamin and calcium levels all help safeguard knee integrity.
Nutrition for Joint Health
Fueling your body with joint-friendly nutrients is a long-term investment. Include foods rich in omega-3 fatty acids (salmon, flaxseed), vitamins C, D, and K, and calcium to keep bones and cartilage resilient.
Hydration is also vital—adequate water intake maintains synovial fluid production, ensuring smooth joint movement ⧉.
Editorial Advice
Caring for your knees isn’t just about avoiding pain—it’s about preserving freedom of movement, stability, and confidence in every step. The varus knee, though often rooted in genetics, doesn’t have to define your mobility or your quality of life. Preventive care and early attention can make all the difference between managing discomfort and enjoying lifelong joint health.
Take, for instance, a 52-year-old office manager from Denver who noticed a gradual outward bow in her legs. Instead of ignoring it, she sought evaluation, started a structured exercise program, and introduced weight management goals. Within six months, her gait had improved, pain levels dropped by nearly 40%, and her confidence returned. That’s the power of proactive care.
Modern rehabilitation centers across the U.S. now combine biomechanical assessment with AI-based gait correction systems, helping patients retrain how they move, step by step. These technologies not only improve physical alignment but also build a sense of control over one’s health journey.
As Reyus Mammadli, a medical consultant, emphasizes: “Every patient who takes ownership of their knee health rewrites their prognosis. Prevention is no longer passive—it’s a personalized, intelligent process.”
Think of your knees as loyal companions: they carry you through life, but they also need your care. Just as you wouldn’t drive thousands of miles without checking your car’s alignment, your knees too deserve regular check-ups, proper ‘fuel’ (nutrition), and timely maintenance.
So, whether you’re a lifelong athlete, a desk professional, or someone simply wanting to walk without discomfort—listen to your knees. Support them with balanced activity, nourishing foods, and expert guidance when needed. Because when your knees move freely, so does your life.