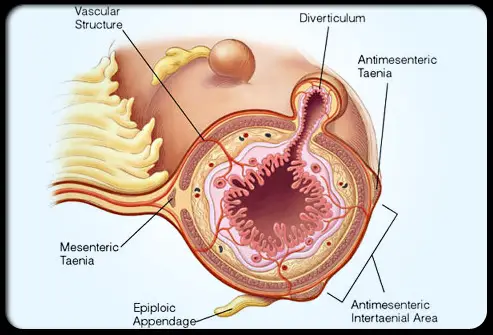
Diverticula are small, bulging pouches that can form in the lining of your digestive system. They are found most often in the lower part of the huge intestinal tract (colon). Diverticula are common, especially after age 40, and seldom cause problems.
Sometimes, nevertheless, several of the pouches become inflamed or infected. That condition is known as diverticulitis (die-vur-tik-yoo-LIE-tis). Diverticulitis can cause severe abdominal pain, fever, nausea and a marked change in your bowel habits.
Mild diverticulitis can be treated with rest, changes in your diet and antibiotics. Severe or repeating diverticulitis may require surgery.
Symptoms of Diverticulitis
The symptoms and signs of diverticulitis include:
- Pain, which might be continuous and persist for a number of days. Pain is typically felt in the lower left side of the abdominal area, however may happen on the right, specifically in people of Asian descent.
- Nausea and vomiting.
- Fever.
- Abdominal inflammation.
- Constipation or, less frequently, diarrhea.
Causes of Diverticulitis
Diverticula normally establish when naturally weak places in your colon give way under pressure. This causes marble-sized pouches to protrude through the colon wall.
Diverticulitis occurs when diverticula tear, leading to inflammation or infection or both.
Risk factors
A number of factors might increase your risk of establishing diverticulitis:
- Aging. The incidence of diverticulitis increases with age.
- Weight problems. Being seriously overweight increases your chances of developing diverticulitis. Morbid weight problems might increase your risk of requiring more-invasive treatments for diverticulitis.
- Smoking. People who smoke cigarettes are more likely than nonsmokers to experience diverticulitis.
- Lack of workout. Vigorous workout appears to lower your risk of diverticulitis.
- Diet high in animal fat and low in fiber, although the function of low fiber alone isn’t clear.
- Specific medications. A number of drugs are connected with an increased risk of diverticulitis, consisting of steroids, opiates and nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin IB, others) and naproxen (Aleve).
Diverticulitis Complications
About 25 percent of individuals with intense diverticulitis develop complications, which might include:
- An abscess, which takes place when pus collects in the pouch.
- A blockage in your colon or small intestine caused by scarring.
- An unusual passage (fistula) in between sections of bowel or the bowel and bladder.
- Peritonitis, which can happen if the infected or swollen pouch ruptures, spilling intestinal contents into your abdominal cavity. Peritonitis is a medical emergency and needs immediate care.
Diagnosis
Diverticulitis is typically diagnosed during an intense attack. Because abdominal pain can indicate a number of problems, your doctor will have to eliminate other causes for your symptoms.
Your doctor will likely start with a physical exam, consisting of examining your abdominal area for tenderness. Women, in addition, usually have a pelvic evaluation to dismiss pelvic disease.
After that, your doctor will likely suggest:
- Blood and urine tests, to look for signs of infection.
- Pregnancy test for women of childbearing age, to dismiss pregnancy as a cause of abdominal pain.
- Liver function tests, to rule out other causes of abdominal pain.
- Stool test, to dismiss infection in people who have diarrhea.
- CT scan, which can indicate swollen or infected pouches and verify a diagnosis of diverticulitis. CT can also indicate the severity of diverticulitis and guide treatment.
Treatment for Diverticulitis
Treatment depends upon the seriousness of your signs and symptoms.
Uncomplicated diverticulitis
If your symptoms are mild, you might be treated at home. Your doctor is most likely to suggest:
- Antibiotics, to treat infection.
- A liquid diet for a few days while your bowel heals. Once your symptoms improve, you can progressively add solid food to your diet.
- An over the counter pain reliever, such as acetaminophen (Tylenol, others).
This treatment is successful in 70 to 100 percent of people with straightforward diverticulitis
Complicated diverticulitis and antibiotics
If you have a severe attack or have other illness, you’ll likely need to be hospitalized. Treatment typically involves:
- Intravenous antibiotics
- Insertion of a tube to drain pipes an abscess, if one has formed
Surgery
You’ll likely require surgery to treat diverticulitis if:
- You have a complication, such as perforation, abscess, fistula or bowel obstruction
- You have had multiple episodes of uncomplicated diverticulitis
- You are immune jeopardized
There are two main types of surgery:
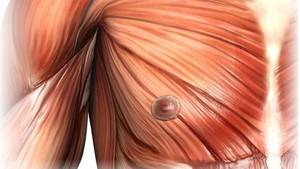
- Main bowel resection. The specialist removes unhealthy segments of your intestinal tract then reconnects the healthy sectors (anastomosis). This enables you to have typical bowel movements. Depending upon the quantity of inflammation, you may have open surgery or a minimally invasive (laparoscopic) procedure.
- Bowel resection with colostomy. If you have a lot inflammation that it’s not possible to rejoin your colon and rectum, the cosmetic surgeon will carry out a colostomy. An opening (stoma) in your abdominal wall is linked to the healthy part of your colon. Waste passes through the opening into a bag. As soon as the inflammation has actually alleviated, the colostomy may be reversed and the bowel reconnected.
Follow-up care
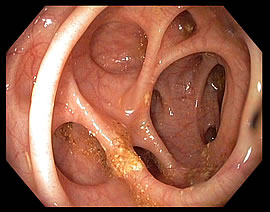
Your doctor might advise colonoscopy 6 weeks after you recover from diverticulitis, specifically if you have not had the test in the previous year. There doesn’t seem a direct link in between diverticular disease and colon or rectal cancer. But colonoscopy– which isn’t possible during a diverticulitis attack– can exclude colon cancer as a cause of your symptoms.
In some cases, surgery is advised. However previous recommendations for surgery based on the number of attacks have been questioned, because the majority of people succeed after two or more attacks. The choice on surgery is a specific one, and is often based on the frequency of attacks and whether complications have happened.
Lifestyle and home remedies
To assist avoid diverticulitis:
- Exercise routinely. Exercise promotes typical bowel function and reduces pressure inside your colon. Try to exercise a minimum of 30 minutes on the majority of days.
- Eat more fiber. High-fiber foods, such as fresh fruits and vegetables and entire grains, soften waste product and help it pass faster through your colon. This minimizes pressure inside your digestive tract. Nevertheless, it isn’t really clear whether a high-fiber diet decreases the risk of diverticulitis. Eating seeds and nuts isn’t associated with establishing diverticulitis.
- Drink a lot of fluids. Fiber works by soaking up water and increasing the soft, large waste in your colon. However if you don’t drink adequate liquid to replace what’s soaked up, fiber can be constipating.
Alternative medicine
Some specialists suspect that individuals who establish diverticulitis might not have enough good bacteria in their colons. Probiotics– foods or supplements which contain useful bacteria– are often recommended as a way to prevent diverticulitis. However that recommendations hasn’t been clinically validated.